Objectives
- Describe ventilation and the involvement of key muscles.
- Describe the relationship between pressure and volume during respiration.
- Measure his/her vital capacity using the wet spirometer and computer-integrated spirometer.
- Define the terms Inspiratory Reserve Volume, Expiratory Reserve Volume, Dead Space, and Residual Volume.
- Calculate the thoracic index, given the appropriate chest measurements.
- Give the composition and temperature variation between inhaled and exhaled air.
- Explain gas exchange at the alveoli and tissue levels.
Introduction
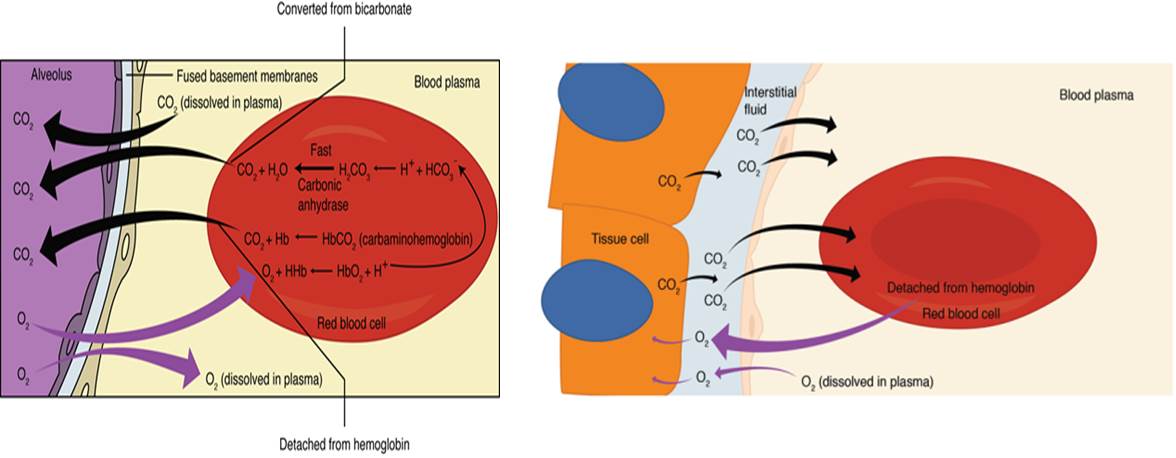
The respiratory system is primarily involved in gas exchange; taking in and delivering oxygen and removal of carbon dioxide. It also plays important role in olfaction and phonation (sound). The entire respiratory process can be divided into external and internal respiration. During external respiration gas exchange takes place between the lungs and blood, while internal respiration involves gas exchange between tissues and cells. Taking in of oxygen or inhalation, involves oxygen being taken in and delivered to the alveoli. Exhalation is the removal of oxygen from the alveoli and delivering it outside the nose. The actual exchange of gases takes place at the respiratory membrane involving the alveoli and capillaries and the capillaries and the interstitial regions of tissues and cells. In both cases gas exchange is as a result of diffusion, where oxygen and carbon dioxide move from areas of high levels to areas or lower lever.
Ventilation or breathing
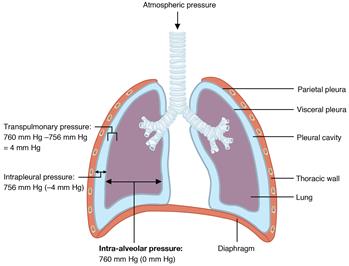
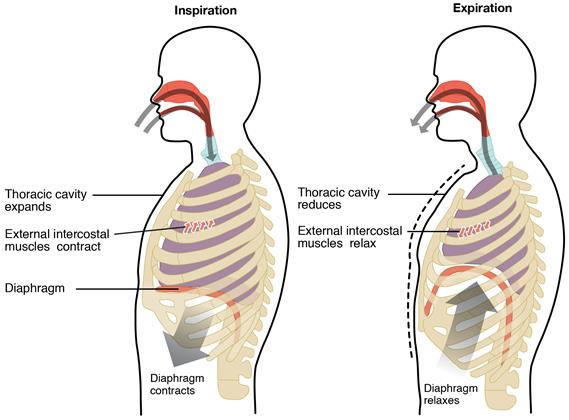
Ability for us to take air into and out of our lungs depends on pressure-volume relationship. According to the Boyle’s law, at a fixed temperature pressure and volume are inversely related. If you increase the volume of a container the pressure within the container decreases (less gas molecules are bumping into each other). Following the laws of physics, air tends to flow from high pressure to low pressure. Breathing involves pressure/volume relationship. Air is taken in, inhalation and breathed out, exhalation, during one breathing cycle or respiratory cycle. Each cycle involves one inhalation and one exhalation. During inhalation the thoracic cavity expands as the diaphragm contracts, increasing the volume of the lungs. The increase in volume also leads to a decrease in pressure in the lungs, intrapulmonary pressure, and pressure in the pleural cavity, intrapleural pressure, slightly below atmospheric pressure which is 750 mm Hg at sea level. Intrapulmonary pressure might be as low as 759 mm Hg while intrapleural pressure may be as low as 754 mm Hg. Air typically moves from high pressure to lower pressure, therefore, air rushes into the lungs from the outside. Conversely, during exhalation the diaphragm relaxes the thoracic cavity contracts decreasing the volume of the thoracic cavity and the lungs. The decrease in volume leads to increase in intrapulmonary pressure causing air to be expelled from the lungs. At the beginning of each cycle, before inhalation begins and after the end of an exhalation both atmospheric pressure and intrapulmonary pressure are equal or at equilibrium, and therefore no air is moved in or out of the lungs.
Gas Exchange
Gas exchange at the alveoli-capillary (external) and tissue-capillary (internal) both occur via simple diffusion. The higher content and pressure of oxygen in the alveoli compared to the capillaries facilitates the diffusion of oxygen into the capillaries, binding to hemoglobin or dissolved in plasma. Likewise the higher content and pressure of carbon dioxide content in the capillaries, as bicarbonate ion, dissolved in plasma or bound to hemoglobin, compared to the alveoli, forces carbon dioxide out of the capillaries into the alveoli. The same mechanism is involved in exchange at the capillary-tissue level. Oxygen, as discussed earlier is mostly carried by hemoglobin. Hemoglobin bound to oxygen is known as oxyhemoglobin. Blood arriving in the lungs has few hemoglobin bound to oxygen. As the blood in the capillaries gets in contact with the alveoli, the high oxygen content and therefore high oxygen partial pressure in the alveoli causes oxygen to diffuse across the respiratory membrane into the capillary and bind to hemoglobin. As oxygen binds to each hemoglobin so to the affinity of hemoglobin for oxygen also increases further increasing the oxygen carry capacity of each hemoglobin. Blood returning to the lung has a higher partial pressure of carbon dioxide than in the alveoli; hence carbon dioxide will diffuse from the blood to the alveoli. The amount of oxygen and carbon dioxide crossing from alveoli to blood and blood to alveoli, respectively, is very similar.
Respiratory Volumes and Capacities
During a typical respiratory cycle, the lungs will take in and expel a certain volume of air. This amount can be increased depending on the activities one is involved in. respiratory air volume refer to the amount of air that can be usually measured using a spirometer. Then normal volume of air inhaled and exhaled during one respiratory cycle is called the tidal volume. This amount is about 500 ml. Other volume that can be measured is the expiratory reserved volume; the amount of air that can be forcefully exhaled after a normal exhalation. These volumes can be used to determine the various lung capacities. Lung capacities, unlike lung volumes, are made up of more than one volumes and usually are calculated using known volumes. The vital capacity is determined by the sum of IRV, ERV and TV. It can also be determined using a spirometer by forcefully exhaling through a spirometer. The normal VC of both male and females are given in tables with standard, predetermined VC. Residual volume is the air left in the lungs after you exhale as much air from your lungs. Functional residual capacity is the volume left after normal expiration.