Learning Outcomes
- Differentiate among arteries, veins, capillaries, and lymphatic vessels as presented in diagrams, photographs and on microscope slides.
- Name the major arteries and veins of the body and the areas which they supply or drain.
- Trace the path of blood from the extremities back to the heart and vice versa.
- Dissect the circulatory system of the fetal pig.
- Identify major organs, arteries and veins in the fetal pig.
- Compare the circulatory system of the fetal pig with that of the human.
- Compare the fetal circulation with that of the adult.
Structure and Organization of Blood Vessels
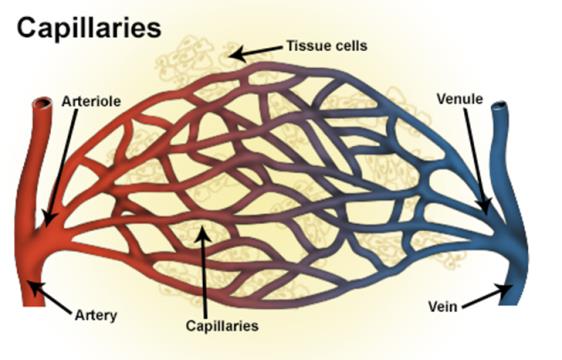
The circulatory system is a closed system, blood remains in and is transported to and from various parts of the body via blood vessels. Blood vessels vary depending on the the size, location and function. Vessels that are closer to the heart tend to have thicker walls than vessels further away from the heart. Ateries are under higher pressure than veins therefore have thicker walls than veins. As stated previously arteries carry blood away from the heart while veins carry blood to the heart. Flow of blood from the heart to tissue flow from elastic arteries, muscular arteries, to arterioles and then to capillaries where exchange of material takes place. From capillaries blood then flows to venules, to medium sized veins and then to large veins.
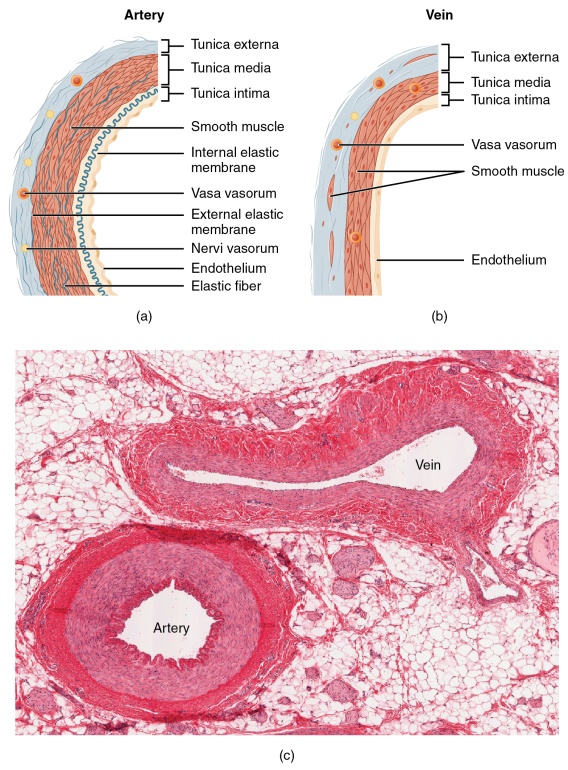
Figure 2. Structure of arteries (a) and veins. (b). Arteries have thicker walls and maintain its round shape compared to veins. (Credit: OpenStax Anatomy and Physiology CC BY 3.0)
Blood vessels have, except capillaries, three layers; tunica intima, tunica media and tunica externa. The tunica intima is the layer closest to the lumen (opening of the blood vessel). In both all blood vessels the tunica intima is made up of a thin layer of endothelium (simple squamous epithelium) on a thin basement membrane, and connective tissue. In arteries, the tunica intima has a thin elastic lamina. Unlike arteries, large veins have valves to prevent the back flow of blood on its way to the heart. In general, blood returning to the heart is also assisted by muscular contractions and pressure changes (thoracic region). The tunica intima is continuous from arteries to veins. Besides forming the inner layer of the vessel, the tunica intima is also very important for processes like clotting, signaling of defense system and inflammation. The next later, the tunica media, is found in all blood vessels except capillaries, is the middle layer made up of smooth muscle cells, elastic fibers called elastin and connective tissue. This layer is responsible for contraction (vasoconstriction) and relaxation (vasodilation) of blood vessels. The tunica externa is the outermost layer and is composed of mainly connective tissue and a layer of elastic lamina. This layer is usually thicker in veins than arteries.
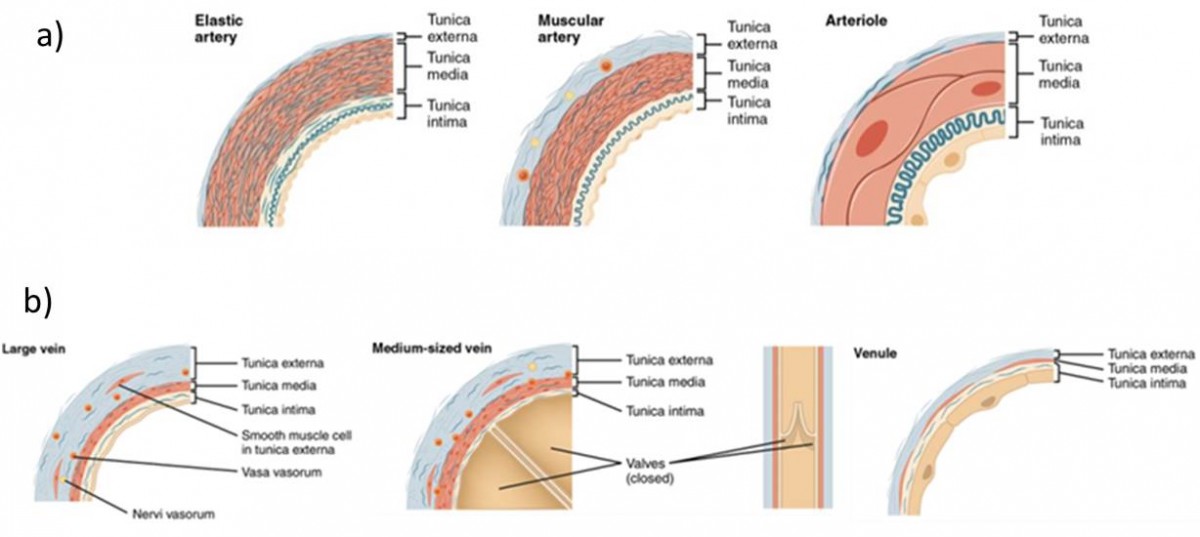
Figure 3. Types of arteries, arterioles, veins and venules. (Credit: OpenStax Anatomy and Physiology CC BY 3.0)
Major Arteries of the body
Neck and Head
Blood leaves the aortic arch and enters the brachiocephalic artery and left common carotid arteries. From the brachiocephalic artery, blood enters the right common carotid and like the left common carotid, continue until they divide into the internal, supplies the brain, and external carotid, supplying the head, face and neck. The left and right vertebral artery, which come from the subclavian arteries and passes through the vertebral foramen and foramen magnum, supplie the brain stem, brain and spinal cord. The vertebral arteries join to form the basilar artery. The basilar artery and the internal carotid arteries anastomose via the posterior communicating artery. This anastomosis together with the anterior cerebral artery and the anterior communicating artery form the circle of Willis. Other arteries supplying the brain include the middle cerebral, posterior cerebral artery and the superior cerebellar artery.
Blood from the head returns to the heart via the left and right jugular veins and the vertebral veins. Blood leaves the brain via the sinuses formed from the outer membrane of the brain, the dura mater, and return by way of the internal jugular veins. From there, blood flows to brachiocephalic veins and empties into the superior vena cava.
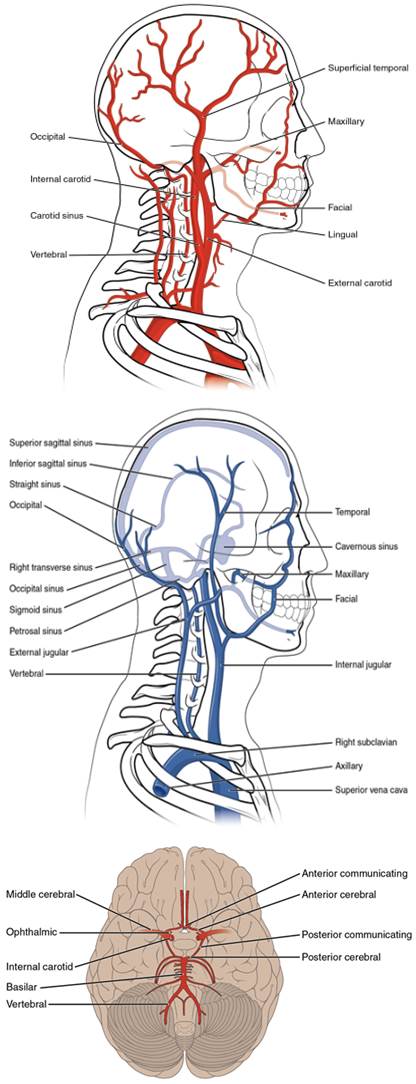
Figure 4. Major arteries and veins of the head, neck and brain. (Credit: OpenStax Anatomy and Physiology CC BY 3.0)
Blood Flow to and from the Upper Extremities
From the aortic arch blood flow to the brachiocephalic trunk (only the right side) and left subclavian artery. The brachiocephalic trunk gives out a branch forming the right subclavian artery. Both subclavian arteries continue towards the arm until at the armpit region where they become the axillary arteries. These axillary will then become the brachial arteries. Several arteries will branch from the axillary arteries feeding the head of the humerus region, the shoulder region and chest walls. The brachial artery supplies most of the brachium. At the elbow, the brachial artery divides into the radial artery and ulnar artery. These arteries will follow the bones corresponding to their names until they fuse at the wrist to form palmar arches and digital arteries.
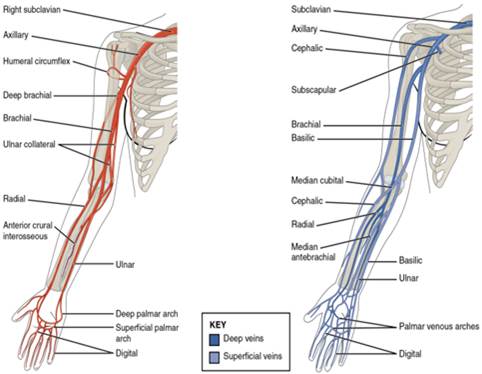
Figure 5. Major blood vessels of the upper extremities. (Credit: OpenStax Anatomy and Physiology CC BY 3.0)
Blood draining from the upper upper limb flow in vessels with similar names and locations as arteries. From plama arches and digital veins to ulnar veins and radial veins, to brachial, axillary veins and then to subclavian veins. However, the basilica vein and cephalic vein do not have corresponding arteries. There is also the superficial vein, media cubital vein, which is used for regularly for collecting blood from individuals. From the subclavian blood flows to the left and right brachiocephalic vein and then to the superior vena cava. Unlike the arterial blood supply which has only one brachiocephalic trunk, the venous system has two brachiocephalic veins.
Blood Flow to and from the Thoracic and Abdomen Region
Blood to thoracic region and lower comes via the descending aorta. In the thorax it becomes the thoracic aorta giving rise to blood vessels supplying some structures and organs in the thoracic cavity and walls of the thorax. These include posterior intercostal arteries, bronchial and mediastinal branches. The internal thoracic arteries and thoracoacromial trunk, branches of the subclavian arteries, supply the most of the thoracic wall. Most Blood returning to the heart from the thoracic region follows the the internal thoracic vein and the azygos vein.
When the thoracic aorta crosses the diaphragm it becomes the abdominal aorta Where it will eventually bifurcate at the level of L4 to form the common iliac arteries. One of the early branches of the abdominal aorta is the inferior phrenic which supplies the diaphragm. The celiac trunk follows and gives rise to the left gastric artery (part of the stomach), the splenic artery (the spleen) and the common hepatic artery (liver, stomach duodenum, pancreas and gall bladder). The next blood vessel is the superior mesenteric artery which supplies the most of the small intestine, pancreas and portion of the large intestines. The renal artery, suppling the kidneys, suprarenal artery (adrenal glands), gonadal arteries (the gonads) and inferior mesenteric (portion of the large intestines), lumbar arteries (lumbar region) are major arteries supplied by the abdominal aorta.

Figure 6. Major arteries (A) and veins (B) of the thoracic and abdomen region. (Credit: OpenStax Anatomy and Physiology CC BY 3.0)
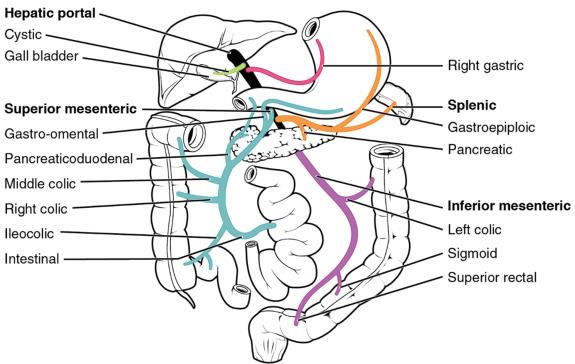
Blood returning from thoracic and abdominal region and returning to the heart has names as their counterpart arteries. These vessels will eventually join the superior (above the heart) and inferior vena cava (below the heart). In addition there are the azygos and hemiazygos veins which drain the right and left intercostal muscles and thoracic region. In the abdomen there is no celiac trunk but there are hepatic arteries returning blood from the liver and GI tract via the hepatic portal system. The hepatic portal system takes blood from the splenic vein, the inferior mesenteric vein and the left gonadal (joins the splenic), the superior mesenteric vein, the gastric veins via the hepatic portal vein. From the hepatic portal vein blood flows to the liver and eventually return to the heart via the hepatic veins and the IVC.
Blood to and from the Lower Extremities
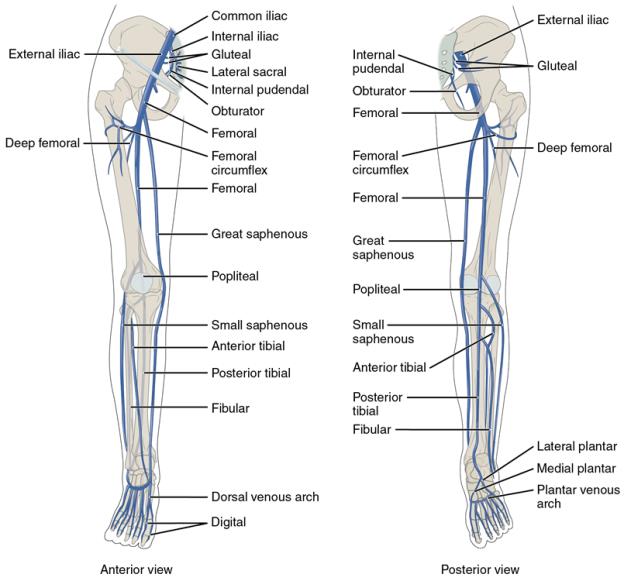
The abdominal aorta bifurcates into the common iliac artery on its way to supplying the lower extremities. The common iliac gives rise to the external and internal iliac arteries. The internal supplies blood to the gluteal muscles. The external iliac becomes the femoral artery supplying the thigh region. At the popliteal fossa of it the femoral becomes the popliteal artery which soon after splits into the anterior and posterior tibial rteries. The anterior supplies anterior tibial region before it forms and becomes the dorsal pedis muscle. The posterior tibial supplies blood to the posterior aspect of the leg. It also gives rise to the fibular branch supplying the lateral aspect of the calf. The posterior tibial splits into the lateral and medial plantar arteries. These will connect with the dorsalis pedis to form the dorsal and plantar arch.
As like other regions of the body, veins of the lower extremities follow counterpart arteries for the most part. Dorsal venous arch to plantar venous arch, anterior and posterior tibial, popliteal, femoral, external and internal iliac vein to right and left common iliac before it makes it to the IVC. Two key differences are the small saphenous vein (superficial region of the leg and foot) and the great saphenous veins (superficial region of the lower limb).
Hepatic Portal System
A portal circulation involves capillary networks connected by a vein. In the case of the hepatic portal circulation, the portal vein connects capillaries in the intestines, spleen, and stomach to capillaries in the liver. This portal system is a direct conduit for blood leaving the GI track. This blood is very rich in nutrients compared to blood from the hepatic artery which is rich in oxygen. The blood making its way to the liver will be processed where excess nutrients will be removed and stored, waste material will be removed, and detoxification of certain substances will take place. Eventually blood will be returned to the IVC via the hepatic veins.
Fetal Circulation
The circulatory system in fetus is slightly different from that of an adult. While the fetus is in the womb, the lungs are collapsed and are not being utilized even if blood must circulate from the right side of the heart to the left side and to be sent all over the body. The placenta is the organ responsible for exchange of nutrients and waste between the mother and the fetus. From the placenta, blood rich in oxygen and nutrients travel, via the umbilical veins, to the ductus venosus and then to the inferior vena cava.
From the inferior vena cava blood goes to the right atrium; however, most blood must bypass the right ventricle and the pulmonary trunk because the lungs are not yet functional. The blood in the right atrium is shuttled to the left ventricle via the foramen ovale, an opening in the interatrial septum. Blood in the right ventricle will eventually make it the pulmonary trunk but will travel to the aorta by a shunt called the ductus arteriosus. From the aorta blood will be delivered all over the body and on return will make its way to the placenta via the two umbilical arteries. After birth these shunts will be closed or collapsed because they won’t be utilized. The foramen ovale will become the fossa ovalis, the ductus arteriosus will be the ligamentum arteriosum, the ductus venosus will be the ligamentum venosum, the umbilical vein will become the ligamentum teres and the umbilical arteries will be the medial umbilical ligaments.
Activity 2 – Special Circulations
Disease and Disorders Involving Blood Vessels
- Peripheral Artery Disease – Narrowing or blockage of peripheral arteries.
- Aneurysm – bulging or widening of arterial wall.
- Peripheral venous disease – damaged or blocked veins.
- Venous thromboembolisms – blood clots in veins
- stroke or Cerebrovascular accident – caused by blockage or damage to arteries of the brain