Learning Outcomes
- Describe the functions of blood.
- Describe the characteristics of blood.
- Identify various components of blood.
- Distinguish between the various blood cells.
- Demonstrate understanding of blood typing.
- Describe some common blood disorders.
1. Introduction
Blood is an integral part of the cardiovascular system. It is an example of connective tissue and like other connective tissues, consists of a cellular component or formed elements and extracellular matrix or plasma. Formed elements include red blood cells or erythrocytes, white blood cells or leukocytes and platelets or thrombocytes. Compared to RBCs and WBCs which are cells, platelets are fragments of cells called megakaryocytes. In any case they are as important as RBCs and WBCs.
2. Functions of blood
Blood perform functions that can be grouped into three types; transport, defense and maintenance of homeostasis.
- Transport – Blood via RBCs transports oxygen from the lungs to body cells and tissues and carbon dioxide from cells and tissues to the lungs for exhalation. Nutrients from the digestive system is transported all over the body while waste materials and byproducts from metabolism to various organs such as the kidney and liver for elimination. Hormones secreted by endocrine glands are released in the blood and transported to different targets all over the body.
- Defense – Our body is defended by the various types of WBCs found in blood. These WBCs act as the armed forces of the body. They try to protect us from microorganisms like bacteria and viruses, and abnormal or cancerous cells, Once these threats are recognized these cells will perform actions to help eliminate them. Platelets are important for blood clotting, a mechanism which, not only prevent excessive bleeding but also helps the healing process after an injury and also aid in preventing further invasion of microorganisms.
- Maintenance of homeostasis – Blood helps maintain overall balance of important molecules and factors needed by the body. These include proteins, electrolytes and water. The body’s pH level is highly regulated and factors in blood help with this regulation. The blood also helps with stabilization of body temperature.
3. Physical characteristics of Blood (see slides)
4. Composition of Blood
4.1 Formed Elements
As indicated above, blood is composed of solid components or formed elements and fluid components or plasma. The formed elements all originate from a common stem cell known as multipotent hematopoietic stem cell, via a process known as hematopoiesis. Hematopoietic stem cell divides, when required, into myeloid stem cell or lymphoid stem cells. Myloid stem cell can give rise to platelets, RBCs, and granulocytes (basophils, eosinophils and neutrophils) and monocytes. The lymphoid stem cells give rise to natural killer cells and B and T lymphocytes. Both monocytes and lymphocytes are examples of agranulocytes.
Figure depicting the production of the various blood cells from the different stem cells.
Blood, when centrifuged (rapidly spun to separate components by density), the top yellowish liquid layer makes up 46 to 60% of blood. The next layer, white in color is composed of white blood cells and platelets. The last red layer is composed of red blood cells. Both the middle or buffy layer and the bottom layer make up 54 to 40% of blood. When blood clots, the fluid component is referred to as serum. Serum, compared to plasma, has little to no clotting factors.
4.2 Blood Plasma (see slides)
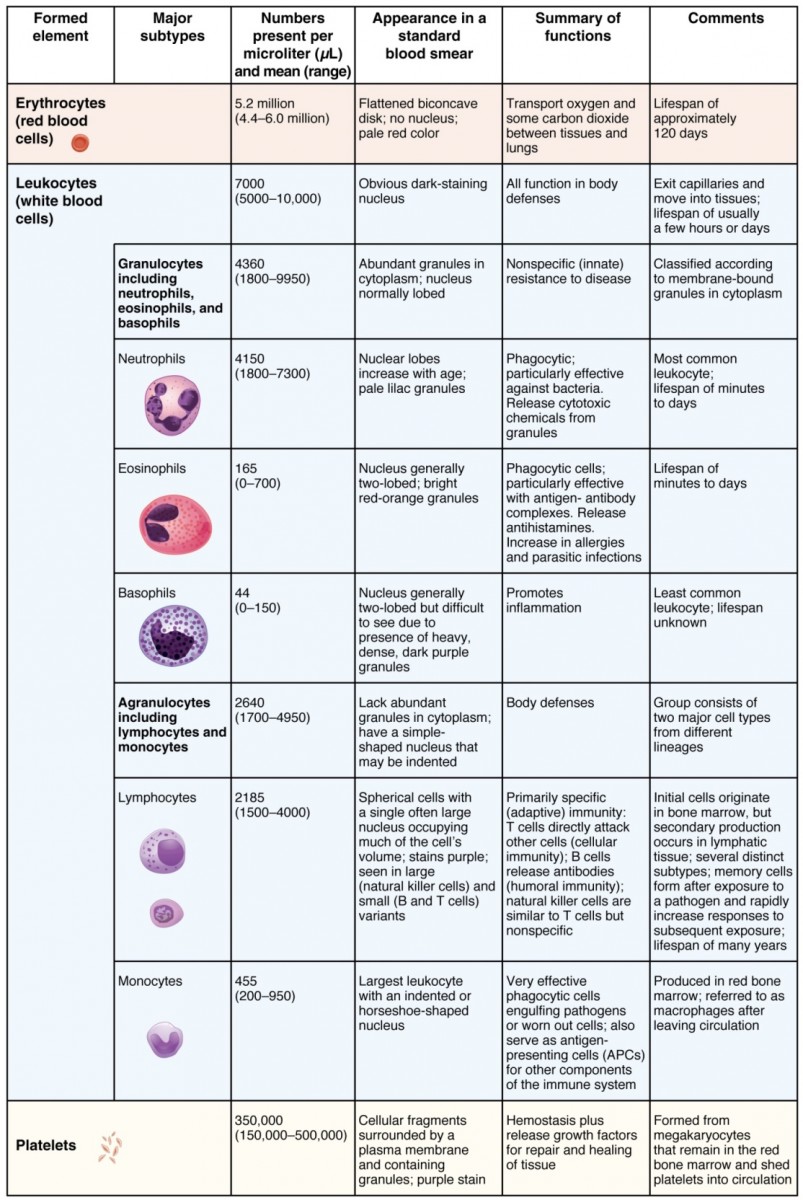
Summary of formed elements in blood
5. Red Blood Cells (Erythrocytes)
Red blood cells make up most of the formed elements. See above. When healthcare professionals are interested in the amount of RBCs in a patient’s blood a hematocrit will be performed and the volume of RBCs is referred to as packed cell volume (PCV). This test will help diagnose anemia, which is a condition where blood lacks oxygen. This lack of oxygen can be as a result of low RBCs, sickle cell or bone marrow disease. Each red blood cell contains about 300 million hemoglobin molecules. Hemoglobin molecules are composed of proteins and iron. Each hemoglobin, Fig. 1 (a), is composed of four chains of proteins or globin bound to a pigment called heme. Each heme, Fig 1(b), contains an ion of iron, which is where oxygen binds to. One oxygen molecule will bind to each iron; therefore one hemoglobin can bind four oxygen molecules. The shape of the RBCs is also import for its function. Normal blood cells are biconcave in shape with few organelles. Having few organelles increases the number of oxygen molecules that can be transported. The shape also allows for these cells to traverse the small diameter capillaries. In sickle cells the shape of the RBCs are crescent shaped or sickled. This makes the sickled RBCs more likely to stick together and block small blood vessels or capillaries. They also carry less hemoglobin and therefore less oxygen.
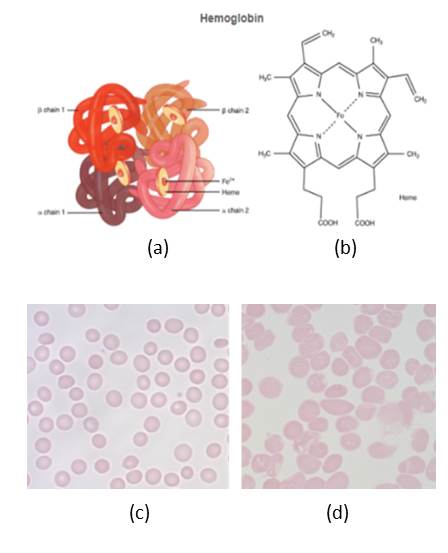
Figure 2. Hemoglobin and RBCs. (a) Structure of hemoglobin molecules. (b) structure of heme. (c) normal RBCs. (d) RBCs from a sickle cell patient. (Panels (a) and (b) credit: OpenStax Anatomy and Physiology CC BY 3.0. Panels (c) and (d) credit: Alcendor CC BY)
6. White Blood Cells (Leukocytes)
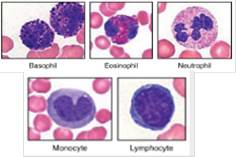
White blood cells can be divided into two major groups; granulocytes and agranulocytes. The pigmented granulocytes have granules hence gran in granulocytes, while the agranulocytes do not necessarily lack granules; the granules are less and are not readily visible. Neutrophils, eosinophils and basophiles are granulocytes, while monocytes and lymphocytes are agranulocytes. In terms of Examine the table below and give the color associated with each of these granulocytes. Both granulocytes and agranulocytes have distinguishing characteristics in terms of color, number and shape of lobed nucleus. The table below provides relevant information for each blood cell. When attempting to diagnose various diseases and infections, a differential WBC count may be required. During the test 100 10 200 WBCs are counted and tallied for each WBC type. The results are compared to normal ranges in order to identify any variation from the norm. Abnormally high WBCs is leukocytosis, while low WBC count is referred to as leukopenia.
Activity 2 – White Blood Cells and Platelets
7. Platelets
Platelets or thrombocytes are important for blood clotting. Remember platelets are not cells but fragments of cells called megakaryocytes, surrounded by plasma membranes. After damage to blood vessel platelets will stick together and also to other factors like fibrin to form a plug to prevent excessive bleeding. They are also involved wound healing and immunity. Abnormally number of platelets is a condition called thrombocytosis, while low number of platelets is called thrombocytopenia.

Figure 4. Blood cells from a blood smear. (Credit: (a) – (c) Alcendor, CC BY (d) Erhabor Osaro CC BY-SA 3.0)
8. Important Tests Using Blood and Blood Components
1) Differential white blood cell count – determine the percentage of various white blood cells in a blood smear. Important for determing infections and leukemia.
2) Hematocrit – Measuring of the percentagve of RBCs in a sample of whole blood (described previously). Blood is centriguge using a heparinized capillary tubes. At the end the amount of RBCs are determined by comparing the results with a microhematocrit reader. Important for diagnosing anemia.
3) Hemoglobin concentration – Measures the amount of hemoglobin in a patient’s blood sample. Methods used include Tallquist Method or a hemoglobinometer. Used for determining anemia.
4) Bleeding time – How long bleeding lasts or how fast bleeding stops. This usually involves capillaries.
5) Coagulation time – Test to measure clotting ability or clotting disorders.
6) Blood typing – Test to determine blood type.
7) Plasma protein tests – detects the total amount of plasma proteins such as albumin, and globulins. Help determine conditions such as rheumatoid arthritis, celiac disease,
8) Thrombin test – measures fibrinogen activity. Important for determining inferited fibrinogen disorders.
Activity 3 – Blood Smear and Differential White Blood Cell Count
8.1 Blood Typing
Blood transfusions are done routinely when patients require blood. It is not common practice to give blood to patients from anyone without having to test for compatibility. One test done to identify compatible blood is blood typing. In this test a donors blood is tested for presence or absence of antigens A and or B. Antigens are molecules or substances the body will build antibodies against because it does not recognize these as belonging to the body. In terms of blood typing, an individual may have antigen A (blood type A), antigen B (blood type B), both A and B antigen (blood type AB) or have none of these antigens (blood type O); hence the term ABO blood group. If incompatible blood types are mixed, these antigens will bind to antibodies present in the blood causing agglutination. The antibodies present are determined by the antigen present. Blood type A will have antibody type B; blood type B will have antibody type A; blood type AB will have neither antibody type A or B and blood type O will have both antibodies type A and B. Blood typing uses these interactions to determine the blood type of a specimen. Blood typing also identify another antigen on RBCs known as the Rh antigen or antigen D. If the Rh antigen is present the blood type is indicated as positive and negative if it is absent. So blood type A+, for example, indicates antigen A and the Rh antigen are present, while A- indicates the A antigen is present but the Rh antigen is absent. The same designation goes for all blood types. One difference with the Rh antigen, antibody against it is only present when an individual who is Rh- is exposed to Rh+ blood. This is known as sensitization. Testing for Rh factor is especially important for mothers who are Rh- and have Rh+ babies (Blood typing – Rh Blood Groups). Statistics of blood types in the US. If a mother who is Rh- has a RH+ baby, the mother’s blood can be exposed to the badies blood leading to the mother making antibodies against the Rh antigen. In subsequent pregnancies with Rh+ babies, the antibodies against the Rh factor can cross the placenta into the baby’s bloodstream destroying the fetuses RBC. This condition is known as hemolytic disease of the newborn.

Figure 8. Summary of blood antigen and antibodies present in plasma. (Credit: OpenStax Anatomy and Physiology CC BY)