Case Study 1: Sleep Apnea
Below is a powerpoint presentation of information on a patient who presented with Sleep Apnea. Included are demographics, all assessments performed on the patient, explanation of the condition, dental hygiene managements, clinical findings, implementation of treatment, and outcomes/ prognosis of treatment. Also, presented here are intra-oral pictures of the patients oral cavity.
Case Study 2: Arestin
V.S. 46yr old South American (Guyanese) woman (Heavy/Periodontal Type II inital visit in 2018 and going down to Medium/Type 2 in 2019) ASA I. BP: 143/86 P: 66 2/27/18, BP: 155/98 P: 67, pt was given referral for BP, which she had taken care of. Patient takes no medications, only modified diet for lowering BP, no allergies or medical conditions present.
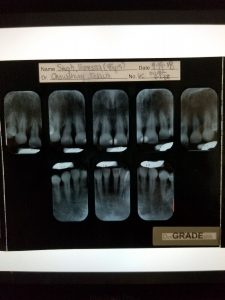
Dental Charting: Missing teeth #4, 18, and 31. Diastemas localized to all maxillary anterior teeth and #24. Composites #8 and 9/L, #14 and 15/MO.
Periodontal Charting: Gingiva was generalized pink with slight inflammation. Localized blunted papilla #6,7,8,24, and 25, and slightly rolled papilla posteriorly. Gingiva is generalized soft, slightly resilient and stippled texture. Patient had periodontal charting done three times with moderate bleeding on probing that decreased on each visit. Along with this, there was generalized attrition present. Patient presented with enough calculus presence to be categorized as a heavy, heavy, then on last visit a medium. Patient was seen by me for all visits and for the first probe readings in 2018, patient had generalized 3-4mm readings, with localized 5-7 mm readings posteriorly. These readings were then generalized 3-4mm, and localized 4-6 mm posteriorly in 2019.
Below is a summary of what was done during all visits in 2019.
Visit 1: All assessments were completed and vitals were taken. Clinical findings were a palpable non-tender left submandibular lymph node, crepitation of the right side of the TMJ with no pain, and slight palatal torus. Class of occlusion I, overjet: 3mm, overbite: 50%. OHI- Recommendation of flossing daily, brushing using Modified Bass method of tooth brushing 2x per day with a soft toothbrush and rinsing with Listerine Antiseptic (10ml for 30 secs) daily. Patient qualified for 16 sites of Arestin on this visit. Upper right quadrant was debrided on this visit.
Visit 2: 1 Bitewing radiograph was exposed on this visit due to evaluating #13 for possible decay. As per the radiograph, no decay was present. Upper right quadrant that was previously scaled was reevaluated for tissue response and any residual calculus. Tissue responded well to treatment and showed a decrease in inflammation, with a slightly tighter feeling to the patient. Plaque Score showed improvement from 1.0 to 0.9. OHI- Reviewed the way patient has been flossing. Debridement of LR, UL and LL quadrants using a combination of ultrasonic and hand scalers. Engine polished using fine grit pumice and application of 5% Fluoride Varnish treatment.
Visit 3: Reevaluation of all quadrants that were scaled to check for tissue response. Patient responded positively to treatment interventions and the tissue showed a decrease in overall inflammation, but was still a bit inflamed. Patient stated incorporating the OHI recommendations everyday since the very first visit. Arestin was placed on 16 sites; 8 placed by me and 8 placed by a fellow classmate.
Sites: 1MB, 2DB, 2DL, 3MB, 5MB, 5ML, 7ML, 7L,12ML, 12L, 12MB, 14ML, 15MB, 15DB, 16MB, 16ML.
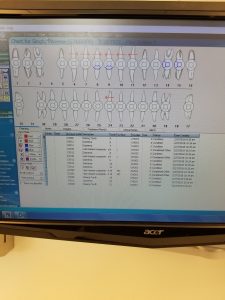
Probe readings before Arestin (as listed per tooth above):
Probe readings after Arestin:
Visit 4: Reevaluation of Arestin sites. After placing Arestin, patient had between 1-2mm pocket reduction in all sites. From the patients first visit in 2018 to the patients last visit in 2019, her pocket reductions decreased significantly posteriorly. The patient stated she was very pleased with all her visits at the City Tech dental hygiene clinic. Not only did the debridement and OHI aid this patient in increasing the health of her oral cavity, but Arestin helped with the extra push to ensure more reduction in her pocket depths.
Case 3:
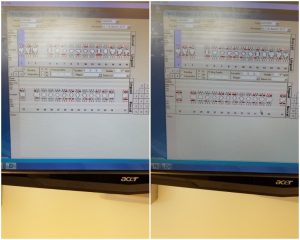
 left is before debridement and right is after debridement
left is before debridement and right is after debridement
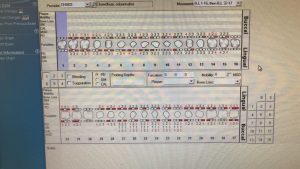
H.I. 22yr old Pakistani woman (Heavy/Periodontal Type II initial visit in 2018 and remaining Heavy/Type II for recare visit in April 2019) Patient complained of mouth feeling irritated and having spontaneous bleeding. ASA I. BP:89/51 P:72 (2018), BP: 86/50 P:93 (2019) Patient takes no medications, no allergies or medical conditions present. Non smoker or drinker. Patient was give referral for active caries.
Dental Charting: Patient has moderate gag reflex, class of occlusion III bilaterally, Underjet 1mm, overbite 0%. Patient has teeth #1 and 16 impacted due to no clinical presentation and no radiographs available during first visit. (At this time radiology department was not available) Occlusal composites present on #2,3,4,13, 18,19, 21 and 31. Several areas of decay included: #7/ML, 10/L, 14/OL, 15/O, 27/D, and decay on #30/MODBL which was so severe that it was partially fractured. All decay impacted patients ability to maintain proper oral home care. Patient complained of malodor and bleeding from mouth upon waking in the morning. In other words, there was bleeding present on her pillow.
Periodontal Charting: Heavy supra and subgingival calculus and periodontal type II. Patient was severely sensitive and did not wish to have any local anesthesia or block anesthesia given. Gingiva was generalized erythematous and inflamed. It was generalized soft and had spontaneous bleeding. Papilla is generalized bulbous, and there is visible plaque with recession on the mandibular anteriors. Severe bleeding on probing and attrition on all canines due to bruxism at night.
Visit 1: (2018): Initial visit. All assessments were completed. For extraoral examination, patient had slight TMJ crepitation on the right side with pain upon opening wide. For intraoral examination, patient had a 2m round aphtous ulcer on her labial mucosa on her lower lip. She had swollen incisive papilla, 3mm round pustule on the left side of her throat, but was not aware of it and had no pain. There was a 1mm bony expansion on the right, lingual side of her mandible near #31. Patients gag reflex created much difficulty to perform assessments, but were completed in a timely manner ensuring as much patient comfort as possible. Every few minutes the patient needed to rinse out due to blood irritating her.
Due to patients gag reflex, need to rinse every few minutes, severe sensitivity and not wanting anesthesia, 4 appointments were needed for thorough debridement while maintaining patient comfort.
Visit 2: Obtained patient consent. Educated patient on oral conditions and importance of proper oral hygiene at home. Taught patient modified Bass technique of toothbrushing in order to remove all plaque from gingival margin. The entire lower right quadrant was debrided and the upper right was started, surpassing the teeth with severe carious lesions. Patient allowed the use of Oraqix. An electric toothbrush was recommended, which patient went out and bought Oral-B Vitality.
Visit 3: Re-evaluated previously scaled quadrants for tissue response. Patient stated feeling tighter on the lower right. Proper flossing technique was taught and told to implement twice daily. Finished debridement of upper right quad and began lower left quad with the use of Oraqix.
Visit 4: Re-evaluated previously scaled quadrants for tissue response. Finished debridement of lower left and upper left quads with Oraqix, subgingival air polish with Glycine powder, applied 5% fluoride varnish, 3 month recare, and gave at home instructions to brush twice daily with 1.1% NaF toothpaste obtained from DDS with referral given to patient, floss twice daily, and use Listerine Total Care (0.05% NaF) twice daily.
April 2019: Recare visit, only one visit needed. Patient stated visiting dental office after referral was given and was told by office staff nothing could be done that day. She was being told her carious lesions were stable at the moment, mostly due to the insurance she had. On this visit, she was given another referral and a list of possible dental clinics from our clinic dental office list. Heavy Perio type II, with moderate BOP. Gingiva was generalized soft with bulbous papilla anteriorly and rolled GM posteriorly. Full mouth debridement was completed using a combination of ultrasonics and hand instruments, engine polish, 5% NaF varnish was applied and patient was placed on a 3 month recare.
This case was new and difficult. The patient was only 21 years old and presented with a mouth with numerous carious lesions that were left untreated. Patient had severe bleeding and it was spontaneous as well. Without touching the patients gingiva, there was blood present just from opening her mouth. She stated having blood present on her pillow when she wakes up in the morning. Patient had a gag reflex which made her need to rinse every few minutes, making it a bit more difficult to scale more than 2 teeth in between rinses. Along with that, she was extremely sensitive which caused her to move constantly and needing to very often. Patient was uncomfortable with her bleeding, her gagging, and extreme sensitivity and still refused any anesthesia; whether local or block due to fear of needles. Severe bleeding, gagging, need for numerous breaks, and extreme sensitivity from a Heavy/Type II with numerous carious lesions made this patient a difficult case for me during her initial visits. However, having finished this patient, I felt much more confident on my clinical skills and I felt accomplished. It was all worth it when the patient thanked me for everything and told me just how much better she felt about her mouth and smile. She stated no longer having blood on her pillow, implementing all the techniques I instructed her to do, and no longer having as much a malodor as before. Now she was constantly smiling and feeling comfortable in herself. She stated even her family began to compliment her on her teeth. Her satisfaction was my satisfaction and complete warmth. I was able to go from needing 4 visits for this patient to completing her in one visit, with no uncomfort to her. My hope is that she will be able to obtain the proper dental care for her carious lesions and continue to keep up with her oral hygiene at home.