-
Criteria for Quadrant scaling and Root planning
It is within the scope of the Dental Hygienist to Assess, Diagnose, Plan, Implement and evaluate. While assessing one has to look at the findings to determine the presence of gingivitis or periodontal disease and decide on the need for quadrant scaling and root planning. Certain criteria is utilized in making this decision and are as follows; the presence and distribution of inflammation, presence of plaque and distribution, amount and distribution of supragingival and subgingival deposits, periodontal probing depths that are not within normal limits, radiographic bone loss and clinical attachment loss. Based on these findings then one is able to determine the need for quadrant scaling and root planning.
Use of Topical versus Infiltration
-
 .
. 
The choice of topical versus infiltration depends on the case. We might have a patient that need infiltration but refuses so we might have to use only topical. It also depends on the treatment needs of the patient. Topical is easily applied but it does not have a long duration and it also creates a slippery working environment. Some patients might have allergic reactions to topical anesthesia.
Infiltration can be considered in cases where there is deep probing depths, 4mm or greater, if there is the need for extensive instrumentation, if there is discomfort that involves the teeth as well as the gingiva, it helps in hemostasis to control bleeding and has long duration of action. The decision depends on the case and the needs of the patient.
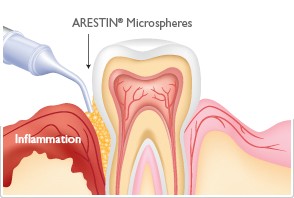
Arestin Placement
- Arestin is appropriate after scaling and root planning when you want reduction in bleeding, improvement in clinical attachment, less inflammation and reduction in pocket depth. It is definitely a choice to consider for cases with moderate periodontitis; probing depths ≥5mm with signs of bleeding upon probing, suppuration. It is also appropriate for patients with Type I gingivitis with moderate to severe inflammation and pocket depth of 4-6mm. For patients with type II (early periodontitis), localized type III; 5-7mm pockets and no pathological mobility, Arestin can be considered.
Below is an actual case of a 52years old, female with Type II localized periodontitis. Initial probing depths 3-6mm, moderate bleeding upon probing and generalized moderate marginal and papillary inflammation. After scaling and root planning Arestin was placed in the following areas:
#3MB-6mm
#3DB-5mm
#12DB-5mm
#13DB-6mm
#14MB-5mm
#14DB-5mm
#14ML-7mm
#13DL-6mm
After 4 weeks reevaluation was done and there was reduction in bleeding and inflammation, probing depths were as follows:
#3MB-4mm
#3DB-5mm
#12DB-5mm
#13DB-5mm
#13DL-5mm
#14MB-5mm
#14DB-5mm
#14ML-5mm
Referrals
When patients are seen they are given referral for any findings that are not within normal limits and for treatment that is beyond our scope of practice. For example; patients with unusual pathology, elevated blood pressure will be given a referral. On the recall visit one must check with the patient if they went to resolve the findings and this is documented in the chart notes.