History of Sleep Disorders
In 1913, French Scientist Henri Pieron authored a book entitled “Le probleme physiologique du sommeil,” which was the first text to examine sleep from a physiological perspective. This work is usually regarded as the beginning of the modern approach to sleep research. Dr. Nathaniel Kleitman, now known as the “Father of American sleep research,” began work in Chicago in the 1920s questioning the regulation of sleep and wakefulness and of circadian rhythms. Kleitman’s crucial work included studies of sleep characteristics in different populations and the effect of sleep deprivation. In 1953 he and one of his students, Dr. Eugene Aserinsky, made the landmark discovery of rapid eye movement (REM) during sleep. Another of Kleitman’s students, Dr. William C. Dement, extended Dr. Kleitman’s path of research. Dement described the “cyclical” nature of nocturnal sleep in 1955, and in 1957 and ’58 established the relationship between REM sleep and dreaming. In 1958, Dement published a paper on the existence of a cyclic organization of sleep in cats. This finding (sleep cycles in species other than humans) created an explosion of fundamental research that pulled together researchers from many different fields electro-physiology, pharmacology, biochemistry for the next 20 years, and led to Michel Jouvet’s identification of REM sleep as an independent state of alertness, which he called “paradoxical sleep.”
In Europe, the discoveries by H. Gastaut and colleagues of the presence of apnea during sleep in a subgroup of “Pickwickian” patients (1965) led to a flurry of investigations of the control exercised by the “sleeping brain” on the body’s vital functions. This type of work eventually led to the new discipline of “sleep medicine.”
Modern Sleep Research
Today, sleep research comprises many different areas: narcolepsy research; sleep and cardio-respiratory research; and studies of pain and sleep, circadian rhythms, shift work and it’s effects on sleep, sleep deprivation, sleep and aging, and infant sleep, to name a few. There are over 200 accredited sleep disorders centers and laboratories in the United States alone, designed to recognize and treat all disorders of sleep. Listed below are some common sleep disorders.
(Dement, Dr. William C. https://web.stanford.edu. 17th December 2016 <https://web.stanford.edu/~dement/index.html#ac>.)
Sleep Disorders
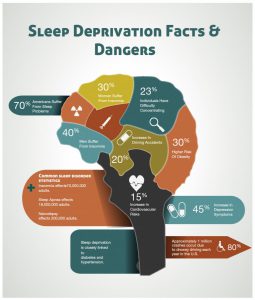
(http://visual.ly/sleep-deprivation. 18th December 2016 <http://visual.ly/sleep-deprivation-facts-dangers>.)
Sleep Apnea
Sleep apnea is a condition in which you stop breathing while asleep. With sleep apnea, your breathing while you are asleep is interrupted by repeated pauses known as apneic events.
Symptoms may also include:
- Being very tired during the day
- Waking up often during the night
- Going to the bathroom often during the night
- Having headaches in the early morning
- Poor memory and difficulty concentrating
- Mood problems
- Weight gain
Sleep apnea can cause serious health problems. It can increase the risk for stroke, obesity, diabetes, heart attack, heart failure, irregular heartbeat, and high blood pressure.
In general, the main risk factors for sleep apnea are male gender, being overweight, and being over 40 years of age. However, anyone can have any of the types of sleep apnea. Strain on the heart. Prolonged suffering from obstructive sleep apnea often results in higher blood pressure and may cause enlargement of the heart, with higher risks of heart attack and stroke. These conditions tend to impair executive functions, alertness, sustained attention, and cognitive performance. A longitudinal study, there were direct link to daytime sleepiness and incidents of road accidents due to sleep apnea.
(Dement, Dr. William C. https://web.stanford.edu. 17th December 2016 <https://web.stanford.edu/~dement/index.html#ac>.)
(Garbarino, Sergio, et al. “Sleep Apnea, Sleep Debt And Daytime Sleepiness Are Independently Associated With Road Accidents. A Cross-Sectional Study On Truck Drivers.” Plos ONE 11.11 (2016): 1-12. Academic Search Complete. Web. 18 Dec. 2016.)
Insomnia
Insomnia is a sleep disorder that is characterized by difficulty falling and/or staying asleep. People with insomnia have one or more of the following symptoms:
- Difficulty falling asleep
- Waking up often during the night and having trouble going back to sleep
- Waking up too early in the morning
- Feeling tired upon waking
Short sleep duration is widely considered to be a risk factor for weight gain, suggesting that patients suffering from sleep disorders are a risk group. A meta-analysis including seventeen cross-sectional studies showed an increased likelihood of obesity.
(Crönlein, Tatjana, et al. “Severe Chronic Insomnia Is Not Associated With Higher Body Mass Index.” Journal Of Sleep Research 24.5 (2015): 514-517. Academic Search Complete. Web. 18 Dec. 2016.)
(Dement, Dr. William C. https://web.stanford.edu. 17th December 2016 <https://web.stanford.edu/~dement/index.html#ac>.)
(Siew, Kong Swee. http://www.macphersontcm.com/. 13th Jan 2016. 18th December 2016 <http://www.macphersontcm.com/single-post/2016/1/13/Sleeping-Disorder-TCM>.)
Causes of Insomnia
Causes of acute insomnia can include:
- Significant life stress (job loss or change, death of a loved one, divorce, moving)
- Illness
- Emotional or physical discomfort
- Environmental factors like noise, light, or extreme temperatures (hot or cold) that interfere with sleep
- Some medications (for example those used to treat colds, allergies, depression, high blood pressure, and asthma) may interfere with sleep
- Interferences in normal sleep schedule (jet lag or switching from a day to night shift, for example)
Causes of chronic insomnia include:
- Depression and/or anxiety
- Chronic stress
- Pain or discomfort at night
(Dement, Dr. William C. https://web.stanford.edu. 17th December 2016 <https://web.stanford.edu/~dement/index.html#ac>.)
(sleepfoundation.org. 18th December 2016 <https://sleepfoundation.org/sleep-disorders-problems>.)
Narcolepsy
Narcolepsy is a neurological disorder that affects the control of sleep and wakefulness. Narcolepsy usually begins between the ages of 15 and 25, but it can become apparent at any age. In many cases, narcolepsy is undiagnosed and, therefore, untreated.
What Causes Narcolepsy?
The cause of narcolepsy is not known; however, scientists have made progress toward identifying genes strongly associated with the disorder. These genes control the production of chemicals in the brain that may signal sleep and awake cycles. Some experts think narcolepsy may be due to a deficiency in the production of a chemical called hypocretin by the brain
What Are the Symptoms of Narcolepsy?
Symptoms of narcolepsy include:
- Excessive daytime sleepiness (EDS): In general, EDS interferes with normal activities on a daily basis, whether or not a person with narcolepsy has sufficient sleep at night.
- Cataplexy: This symptom consists of a sudden loss of muscle tone that leads to feelings of weakness and a loss of voluntary muscle control. It can cause symptoms ranging from slurred speech to total body collapse, depending on the muscles involved, and is often triggered by intense emotions such as surprise, laughter, or anger.
- Hallucinations: Usually, these delusional experiences are vivid and frequently frightening. The content is primarily visual, but any of the other senses can be involved.
- Sleep paralysis: This symptom involves the temporary inability to move or speak while falling asleep or waking up. These episodes are generally brief, lasting a few seconds to several minutes. After episodes end, people rapidly recover their full capacity to move and speak.
How Is Narcolepsy Diagnosed?
A physical exam and exhaustive medical history are essential for proper diagnosis of narcolepsy. However, none of the major symptoms is exclusive to narcolepsy. Several specialized tests, which can be performed in a sleep disorders clinic or sleep lab, usually are required before a diagnosis can be established.
(Dement, Dr. William C. https://web.stanford.edu. 17th December 2016 <https://web.stanford.edu/~dement/index.html#ac>.)
Sureshbabu, Sachin, Abdul Muniem, and Manvir Bhatia. “Diagnosis And Management Of Narcolepsy In The Indian Scenario.” Annals Of Indian Academy Of Neurology 19.4 (2016): 456-461. Academic Search Complete. Web. 18 Dec.
Sleep and Circadian Rhythm Disorders
Circadian rhythm disorders are disruptions in a person’s circadian rhythm — a name given to the “internal body clock” that regulates the (approximately) 24-hour cycle of biological processes.
What Causes Circadian Rhythm Disorders?
Circadian rhythm disorders can be caused by many factors, including:
- Shift work
- Pregnancy
- Time zone changes
- Medications
- Changes in routine such as staying up late or sleeping in
- Medical problems including Alzheimer’s or Parkinson disease
- Mental health problems
How Are Circadian Rhythm Disorders Treated?
Circadian rhythm disorders are treated based on the kind of disorder diagnosed. The goal of treatment is to fit a person’s sleep pattern into a schedule that allows him or her to meet the demands of their lifestyle. Therapy usually combines proper sleep hygiene techniques and external stimulus therapy, such as bright light therapy or chronotherapy. Chronotherapy is a behavioral technique in which the bedtime is gradually and systematically adjusted until a desired bedtime is achieved.
(http://www.webmd.com/. 18th December 2016 <http://www.webmd.com/sleep-disorders/>.)
(Dement, Dr. William C. https://web.stanford.edu. 17th December 2016 <https://web.stanford.edu/~dement/index.html#ac>.)
REM Sleep Disorder
Normal sleep has two distinct states: non-rapid eye movement (NREM) and rapid eye movement (REM) sleep. NREM sleep is divided into four stages. During REM sleep, rapid eye movements occur, breathing becomes irregular, blood pressure rises, and there is a loss of muscle tone (paralysis). However, the brain is highly active, and the electrical activity recorded in the brain by EEG during REM sleep is similar to that recorded during wakefulness. REM sleep is usually associated with dreaming. REM sleep accounts for 20%-25% of the sleep period what we call “sleep” involves transitions between three different states: wakefulness, rapid eye movement (REM) sleep, which is associated with dreaming, and non rapid eye movement (N-REM) sleep. REM sleep is important because it is the restorative part of our sleep cycle. Typically, you begin the sleep cycle with a period of non-REM sleep followed by a very short period of REM sleep. The period of non-REM sleep is made up of stages 1 to 4. Each stage can last from 5 to 15 minutes. A completed cycle of sleep consists of a progression from stages 1 to 4 before REM sleep is attained, then the cycle starts over again.
Causes of REM Sleep Disorder
The exact cause of REM sleep behavior disorder (RBD) is unknown, although the disorder may occur in association with various degenerative neurological conditions such as Parkinson’s disease, multisystem atrophy, diffuse Lewy body dementia, and Shy-Drager syndrome. In 55% of persons the cause is unknown, and in 45%, the cause is associated with alcohol or sedative-hypnotic withdrawal, tricyclic antidepressant (such as imipramine), or serotonin reuptake inhibitor use (such as fluoxetine, sertraline, or paroxetine) or other types of antidepressants (mirtazapine).
Diagnosis of REM Sleep Behavior Disorder
Because a number of parasomnias may be confused with RBD, it is necessary to conduct formal sleep studies performed at sleep centers that are experienced in evaluating parasomnias in order to establish a diagnosis. In RBD, a single night of extensive monitoring of sleep, brain, and muscle activity will almost always reveal the lack of muscle paralysis during REM sleep, and it will also eliminate other causes of parasomnias.
(sleepfoundation.org. 18th December 2016 <https://sleepfoundation.org/sleep-disorders-problems>.)
(Dement, Dr. William C. https://web.stanford.edu. 17th December 2016 <https://web.stanford.edu/~dement/index.html#ac>.)