Case 1
Patient is 30 years old, Hispanic male. He presented with severe erosion of his maxillary lingual sextants due to nutritional habits and severe generalized attrition. Patient also has multiple caries lesions. Patient was diagnosed as a Heavy- Type I, localized Type II perio case. Generalized BOP and sensitivity.
The patient was treated with 4 quadrant SRP and administered 5% Varnish. OHI and nutritional habits discussed. Brushing technique demonstrated, Fluoridated toothpaste and mouthrinse recommended. Referral given for general dentist for occlusal guard and caries evaluation.
Journal
Demographics:
Patient is J.R. age 30, heavy/type I, ASA I
Assessment:
Patient has nothing significant in medical history to report. His vital signs were within normal limits BP 134/86 Renin Angiotensin System and pulse was 93.
Patient is non-smoker. No premedications required. No systemic conditions. No allergies.
No medicines are currently being taken.
Oral Pathology:
EO/IO no significant findings, however linea alba present bilaterally. Patient is a cheek biter. Red nodule approx 1-2mm is present on the right buccal mucosa. Patient stated it has been present for a couple days, it doesn’t bother him. Admits his bad habit in stressful situations. Also had a cracked right comissure on the day of the initial appointment. On his re-visit appointment the lesions were within normal.
Dentition:
Patient has missing tooth #12. Patient had a retained root on #2 with partially broken crown, however had #2 recently extracted on 3/11/2015. Extraction site was successfully healing. Multiple areas of suspicious decay. Referral for evaluation of the active carious lesions given. Patient’s class of occlusion is I – bilaterally. Attrition present on #6-11, #22-27. Erosion on #6-11, #22-27. Absence of abfraction, abrasion.
Periodontal:
During gingival assessment generalized minimal to moderate inflammation on the attached gingiva was noted, mainly found on maxillary/mandibullar posterior teeth. Pink color, soft, bulbous. Stippling and pink color present on the rest non affected areas. During periodontal evaluation patient was found to be a Type I with early periodontitis and probing depths ranging from 2-7mm. with the absence of recession. However patient had generalized sensitivity during the treatment. Patient was recommended use of “Sensodine” dentifrice for the sensitivity elimination.
Oral Hygiene:
During the initial visit plaque score indicated 1.2 – which is an indication of fair OH. Patient had generalized subgingival calculus, presence of plaque and biolfilm. Patient last dental visit was back in 2009, and doesn’t recall if he had a prophylaxis done ever in his life.
Patient being asked to demonstrate the brushing technique and apparently he was using horizontal method, heavy strokes. I explained to a patient that eventually it will cause enamel abrasion and gingival recession. I showed the patient the correct brushing technique – modified Bass method and use of light strokes.
The patient also has erosion on the linguals of #6-11, #27. His diet contains of acidic products like orange juices, beer, cultural cuisine contained lemon/lime juices. I recommended use of fluoride contained mouth rinses and re-mineralize the enamel and watch of the nutrition.
On his re-visit appointment, the plaque score was 1.5 within fair indication. Patient has begun using powered toothbrush.
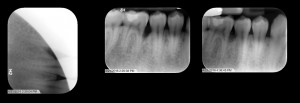
Radiographs:
Patient had had his radiographs taking back in 2009. I took 4 sets of bite-wings on 2/27/2015 during radiology lab class, which revealed absence of bone loss however presence of caries lesions.
Treatment management:
The patient was very sensitive, was not able to tolerate the pain. I had to administer an Oraquix, which contains 2.5% lidocaine and 2.5% of prilocaine. I was using 1 carp on almost every visit. Patient got 4 quadrants of debridement. Ultrasonic cavitron and hand instruments used. Selective polishing and 5% neutral sodium fluoride Varnish administered. Was recommended of rinsing with Baking soda and Fluoridated mouth rinses.
Evaluation:
Patient became more interested in oral hygiene care. He even got a powered TB by my recommendation. He started flossing and using mouthrinses as well. I kept him encouraged and told him that his bleeding and inflammation had reduced during my re-evaluations. We were going over the brushing and flossing technique each visit. He was very happy to hear and see that his oral care was making a significant difference.
Reflection:
The patient didn’t know anything about the teeth care, before I introduced my patient to the oral hygiene science and brought him to clinic. He had to learn a lot about the teeth. Every visit I was giving him OHI instructions, evaluating his home care and introducing him to the new technique and methods of brushing, flossing, tongue cleaning. The patient was willing to learn and improve his oral hygiene care and change his nutritional habits. Overall the patient was compliant with his home care and continued to come to every appointment so I believe despite his resistance, he did see a difference in his oral health. He even went to a dentist for caries evaluation. The dentist extracted tooth #2 and filled tooth #31 MOD composite filling. Also got his occlusal guard made and wears it every night. The patient definitely needs more teeth to be filled. It is still being in process.
Case #2
Patient is 64 years old, Arabic female. Chief complaint: pain on #14, teeth mobility. Diagnosis: Perio Type III, localized IV. Generalized heavy deposits, plaque/biofilm. Last dental hygiene visit 2 years ago. Treatment rendered: OHI discussed: brushing twice a day, use of proxy brushes demonstrated, use of Chlorhexidine 0.12% recommended. 4 quadrants of SRP completed- ultrasonic cavitron, hand instruments. Local anesthesia administered. Patient was referred to periodontist for further evaluation.
Case #3
19 year old African-American male. Light case value. Pocket depths 1-3mm, localized 7mm. After exposing 4 BW and Panoramic Xray, the faculty and I detected juvenile periodontitis and severe vertical bone loss on mandibullar first molars with the pocket depth 7-8mm. The patient was referred to Columbia University College of Dental Medicine for Periodontal evaluation. http://dental.columbia.edu/division/division-periodontics. He got a surgery done recently and feels great about it and appreciates coming to our clinic.