Patient Profile
- Mister C. is a 25-year-old Hispanic male who came for a dental checkup and teeth cleaning.
- C. is a full-time business student. He is divorced and he has a 6-year-old daughter. In order to support himself and to help out his daughter, Mr. C. works part-time in an Italian restaurant as a bus- boy. He currently does not have a dental insurance, therefore he has to pay out-of-pocket for any medical or dental care.
- His last dental exam, as well as last oral hygiene service, were in November 2015
- Last dental X-rays were taken in October 2015. Panoramic radiographs were exposed at this time
- When interviewed, Mr. C. reported using medium bristles manual toothbrush with horizontal scrub- brushing strokes. Patient also emphasized to brush his teeth once or twice a day with anti-cavity Colgate toothpaste. Mr. C. said that he likes to use toothpicks after a meal sometimes and Listerine Zero once a day for a fresh breath. In addition to that, Ms. C. confessed that he does not floss and he does not use any tongue cleaner
Chief Complaint
- Patient states that “I am here to clean my teeth and to improve the bad breath that annoys me a lot”.
- Overall he truly believes that his teeth are in a pretty good shape and the only problem he has is a bad breath
- C. would like to get his teeth cleaned and to improve his breath because he feels embarrassed to kiss his girlfriend sometimes. Also, his bad breath makes him feel less confident in public.
Health History Overview
- Blood Pressure 129/85, pulse 85, ASA II
- Medical Conditions:
- Smoker
- Patient states he does not have any systemic conditions or diseases. However, severe gingival inflammations, extreme marginal redness, gingival enlargement and heavy bleeding upon probing and exploring clearly signal about the presence of some systemic condition that patient is not aware of or he just hides the truth. Patient presented with a very pronounced gingival erythema and a distinct red marginal bend around the free gingival margin that did not improve and did not respond well to a conventional treatment with scaling and root planning or hygiene control. Upon thorough assessment and consultation with various faculties, it has been found that Mr. C. has Linear Gingival Erythema.
- Linear Gingival Erythema has been often observed in patients with HIV
- Current medication:
- Patient reported to do not currently take any medications, supplements, vitamins, over-the-counter products, herbal supplements etc. Patient said he does not have any allergies.
Explanation of Condition
Linear Gingival Erythema
Linear Gingival Erythema (LGE) has very specific features. Linear Gingival Erythema is a gingival condition usually found in immunosuppressed people. Originally LGE was directly linked with HIV-positive patients, that is why it was called HIV-associated gingivitis (HIV-G). However, some studies have shown that LGE can also occur in HIV-negative patients, therefore it is no longer named HIV-Gingivitis. The clinical feature of LGE is a distinct red band about 2 to 3 mm in width around the free gingival margin.
According to the American Academy of Periodontology Linear gingival erythema has been classified as a disease of fungal etiology. The lack of response of Linear Gingival Erythema to oral hygiene measures and conventional periodontal therapy is important for its diagnosis.
Dental Hygiene Management
- Different oral lesions and gingival conditions may represent the early signs of HIV infection. Therefore, dental hygienists should be aware of it. Dental hygienists should be alert when they see Linear Gingival Erythema (LGE), because it is very often associated with HIV. Patient who is present with LGE should be referred to other medical specialists for further diagnosis and management.
- Linear gingival erythema (LGE) has a poor response to plaque removal, oral hygiene, and chlorhexidine rinses in comparison with a typical gingivatis.
- Vacuum-formed trays can be made for the patient with LGE in order to hold the antifungal medicament against the infected tissue. If an infection is persistent and does not resolve in 2 weeks, patient should be referred to the physician for prescription of systemic antifungals such as ketoconazole, fluconazole or itraconazole.
- If fluconazole-resistant forms of candidiasis are present, a mouthwash that contains ketoconazole should be used for the treatment.
COMPREHENSIVE ASSESSMENTS
Summary of clinic findings
- Extraoral/Intraoral Examination: No Significant Findings
- Occlusion: bilateral class I occlusion, Overjet is 4mm, Overbite is 80%
- Dental:
- No restorations
- #17, #32 have suspicious caries lesions on the buccal side, patient was given a referral to a dentist for a further evaluation
- Malposition/crowding of central mandibular incisors #24-25
- #7, #10 are microdonts
- Attrition is present on #6-11, #22-27
- No erosion, no abrasion, no abfraction
- Deposits:
- Generalized extrinsic yellow stains due to smoking
- High amount of biofilm
- Generalized extra heavy supra and subgingival calculus
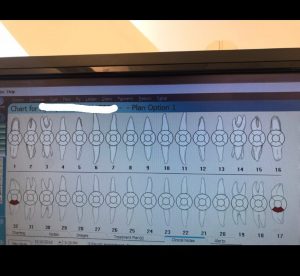
Dental charting
Gingival Description & Periodontal Status
- Gingiva is generally pink with a distinct red band about 2 to 3 mm in width around the free gingival margin. Gingiva is edematous, bulbous, spongy, very inflamed, blunted interdental papilla, generalized marginal redness, gingiva is not firm, not resilient, not stippled.
- Active perio type III, localized IV
- Generalized heavy BOP
- Generalized 5-6 mm Pockets with localized 7-8 mm pockets
- No furcation involvement
- No recession
- No mobility
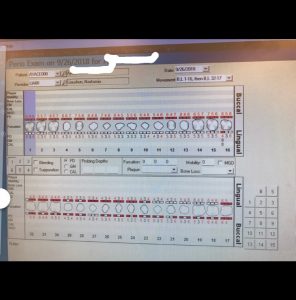
Periodontal Charting
Dental Hygiene Diagnosis
- Periodontal diagnosis
Patient presented with type III (localized IV) active periodontitis due to generalized 5-6 mm probing depths (localized 7-8 mm), extreme gingival inflammation and heavy BOP
- Risk for caries
Patient is at a moderate risk for caries due to several risk factors. Patient does not have a dental home, he does not receive regular dental care, he has inadequate oral hygiene. Moreover, patient has 2 new caries lesions in past 36 months, visible plaque, crowding and poor hygiene habits.
Implementation -Treatment
Preventive services:
-
- The plaque index for the initial visit was 2.6 (poor). The biofilm was covering more than three quarter of the tooth surface. Revisit plaque score was 2.4 and the final plaque score was 2.3 (slightly better, but still very poor). Patient said that he wanted his plaque score to be better and he will keep working on improvements, because he is really interested in better results.
- Based on the findings, I first taught my patient a modified Bass tooth brushing technique. Then, on the next visit, I reviewed with the patient previously taught tooth brushing method and I introduced flossing. Then, when patient came back both previously taught methods were reviewed, corrected and adjusted and patient was advised to keep using them in order to master his skills and to improve the results. On the last visit patient was advised to try an electric toothbrush for better biofilm removal results.
- At the end of the treatment 5% NaFl varnish was applied, post-treatment instructions were given to the patient.
- Patient was advised to use soft bristles manual toothbrush ( or an electrical toothbrush) twice a day with any Fluoride containing toothpaste, to floss twice a day, to use Listerine antiseptic 20 ml (4 teaspoons) for 30 seconds twice a day and to use a tongue cleaner at least once a day
- Debridement performed:
- Patient had a very tenacious thick layer of calculus deposit that encircled every tooth surface. Calculus was so tenacious that it was incredibly hard to remove it from the tooth. First of all, ultrasonic scaler was used but most calculus still did not come off. After that, hand instruments were applied for successful completion of the removal process.
- Working on this patient was very challenging for me. Tenacious calculus, deep pockets, a lot of blood and inflammation slowed down the cleaning process and required a lot of efforts and diligence to finish.
- Advanced fulcrum techniques such as cross arch fulcrum, opposite arch fulcrum, chin-cup technique were used for easier access, better stability of instrumentations and more efficient calculus removal process.
Referrals
- Patient was given a referral to a dentist for further evaluation of suspicious carious lesions on the buccal surface of #17 and # 32.
- Patient was also referred to a physician and a periodontist due to severe marginal gingival erythema and inflammation. Patient was advised to perform a complete blood count (CBC) test and to test his oral flora for microbial prevalence
Final Reflection
- In my opinion, almost everything went well and worked pretty good for this patient. Patient was open to all my recommendations and suggestions and he was ready to try and to learn new things and to change his oral habits. Patient was very interested in a learning process and he was attentive to details. Moreover, patient was willing to come as many times as it is needed for the completion of the cleaning process. Patient refused to use any anesthesia, he said: “It is just teeth cleaning, I am a man, I can handle it”. He tolerated pain really well and he never complained.
- He really liked modified Bass tooth brushing technique that I taught him. He said it feels unusual and very different from the scrub-brushing method that he applied before. He found it beneficial and he emphasized that his teeth feel cleaner after that. He also incorporated a floss in his oral hygiene routine and I was really proud of him, because he never used a floss before.
After I cleaned half of the patient’s dentition, I showed him the result. He was very excited to see how his teeth look without any deposits and he was amazed at how smooth the teeth surfaces became. He also noticed that when I was removing the calculus from his teeth, it smelled very bad and unpleasant. After that, patient said he wished calculus would never form in his mouth again and he would try to do his best in order to prevent or slow down its formation.
- Nothing really went wrong during the treatment process.
- The only thing that made my work on that patient harder is that patient was not able to come to the clinic every week. He was scheduling his appointments in 2 weeks interval and every single time he came back he had newly formed calculus deposits all over his mouth. So before start working on a new quadrant, I had to remove new calculus formation from previously scaled areas again and again.
- When this patient came for the first time, we just start using an ultrasonic, so my technique was not as good as I wish it was. So it took me a long time to remove calculus from his teeth. I was afraid to use ultrasonic, because I was not that good at it and I was scared to hurt the patient or myself as well as to cut patient’ gums. Therefore, I did not apply it efficiently. My hand instrumentation helped me a lot, however, calculus was so tenacious, that I had to do many strokes in order to remove all deposits from the patient’s teeth. As a result, my instruments became dull super fast and I had to stop many times and to sharpen them over and over again.