Case Study 1.
Patient Profile
- Ms. K is a 26 years old African-American, single, female
- Middle class lives in New York with her boyfriend. Has an associate degree in arts, but currently babysitting. Has no dental insurance and has to pay out-of-pocket for care.
- Her last dental exam was on 9/5/18 for a yearly check-up. Never had any hygiene services done before. Full mouth radiographs were taken in October/2017.
- Patient states brushing with an electronic toothbrush once a day for 2 minutes with Colgate desensitizing toothpaste and using floss picks 2-3 times a week, Crest mouthwash 2 times a day.
Chief Complaints
- The patient states that “My bad breath bothering me and also gums bleed a lot.”
- She has heavy deposits on all of her teeth.
- Ms. K would like to get her teeth cleaned so she would not need to carry mouthwash with her all the time.
- She is also concerned about her teeth appearance.
Health History/Assesment/Conditions
Blood Pressure: 160/117, Pulse 77, ASA III
Medical Conditions: Dialysis Patient
Current Medications:
- Heparin (anticoagulant): right before dialysis procedure to prevent deep vein thrombosis. Routine hemodialysis requires anticoagulation with heparin to prevent clotting in the extracorporeal circuit. Because patient responses to heparin differ markedly, the doses required to achieve suitable anticoagulation must be determined on an individual basis.
- Calcium Acetate: during meal time for hyperphosphatemia (reason: too much phosphate in the blood). Phosphate binders, including non-calcium-based phosphate binders and calcium-based phosphate binder, are widely used to lower serum phosphorus levels in CKD (Chronic Kidney Disease) patients and prospective cohort study proved that treatment with phosphorus binders was independently associated with improved survival among incident hemodialysis patients.
- Nifedipine (Calcium Channel Blocker): 30 mg (1 tablet) once a day in the morning for hypertension. Results show that oral Nifedipine is effective in rapidly reducing blood pressure during or following hemodialysis.
- Patient is on dialysis 3 times per week (Mon. Wed. Fri).
The condition is a result of an end stage renal failure – Stage 5 End Stage Chronic Kidney Disease (CKD) (GFR <15 mL/min) which was diagnosed at the age of 10. In children, genetic causes account for the greatest number of cases. Had multiple (four) kidney transplants in the past which were not successful
Signs and Symptoms:
- Ø high blood pressure readings due to excess fluid in the body;
- Ø decreased urinary output;
- Ø swelling due to fluid retention;
- Ø nausea;
- Ø fatigue
- Ø shortness of breath
- Ø too much acid in blood tissues.
Chronic kidney disease (CKD) usually gets worse slowly, and symptoms may not appear until your kidneys are badly damaged. In the late stages of CKD, as you are nearing kidney failure (ESRD), you may notice symptoms that are caused by waste and extra fluid building up in your body. These patients require special attention with regard to bleeding tendencies, risk of infection, xerostomia and multiple medication use.
Dialysis patients may form calculus more rapidly than healthy individuals possibly due to high salivary urea and phosphate levels. Elevated parathyroid hormone synthesis is also common in ESRF which causes accelerated bone loss. This may also exacerbate periodontal disease. Transplant patients who are immunosuppressed often experience a change in oral flora. This can predispose the patient to oral candidiasis. In addition, cyclosporine and calcium channel blockers are known to contribute to gingival hyperplasia, which is exacerbated by poor oral hygiene.
The main oral health problem experienced by renal patients is xerostomia. This is a result of several factors which include multiple medications, restricted intake of fluids and diabetes, which many renal patients suffer from. Xerostomia may also predispose the patient to caries, mucositis and oral infection as the protective factors in saliva are not present.
Keeping a healthy smile when you have kidney failure can take some extra effort. The type of treatment you choose can affect the health of your teeth and gums. In turn, your oral health can have a positive impact on the rest of your body.
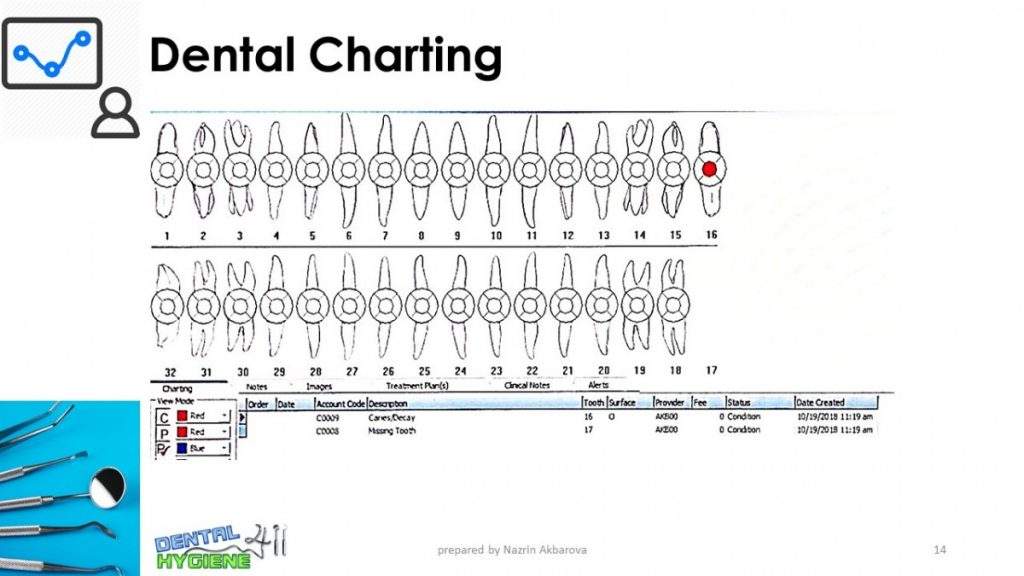
Clinical Findings
Extraoral Examination: Patient has a scar under the left side of her nose flares. According to the patient she fell after dialysis procedure due to dizziness. Right ear has a tear.
Intraoral Examination: No significant findings.
Occlusion: Class I; Moderate Overbite
Dental: Malposition/minimal crowding central and lateral mandibular incisors.
Deposits:
- Generalized light yellow stains
- Generalized severe supra/subgingival calculus


The patient presented with active periodontal status: Type II.
Gingival description: Gingiva is generalized erythematous and enlarged; papilla is inflamed, bulbous, leathery and shiny.
Generalized chronic slight periodontitis
Generalized severe BOP
Radiographic evidence of localized bone loss around tooth #24
Localized moderate recession on teeth # 22, 24, 25, 27
No clinical or radiographic evidence of furcation present.
Localized mobility on tooth # 24
Treatment
- Preventive Services:
- Using electronic toothbrush twice a day for 2 minutes, flossing once a day with regular floss doing a “C” shape.
- Using Listerine antiseptic once a day.
- Fluoride Varnish ( 5% Sodium Fluoride) for dentinal hypersensitivity due to gingival recession.
- Reducing frequent sugary drinks. Removing totally is planned.
- Debridement Performed:
- Debridement performed by using both Ultrasonic and hand instruments.
- Prophylaxis treatment rendered as well as applying fluoride varnish.
- Remembering advanced fulcrum techniques, root morphology, and types of strokes, as well as being knowledgeable about hand instruments were crucial in treating my patient.
- The patient was using Heparin medication for her dialysis catheter, which made her blood very thin and created an additional challenge during debridement in the form of profuse bleeding. The amount was so profound that the teeth were almost unseen.
- Another complication during the treatment was caused by Anesthetic. Due to high blood pressure, we were not able to use Epinephrine and replaced it with Carbocaine. But its effect was withering away rapidly and the sense of pain was coming back soon.


Click the following link to download/preview the full Case Presentation File in PDF format:
Nazrin Akbarova – Case Presentation
Case Study 2: Arestin Placement

Patient Profile:
W.R. 53 years old, African-American male. No systemic diseases, no medications, no allergies, non-drinker, non-smoker. Past history of periodontitis.
Dental Cleaning was performed 1 year ago.
Medium/Type III.
Treatment:
Arestin was performed on the following teeth:
#15B,
#18M,
#18D,
#19M
Probing depth was 6mm on the surfaces where Arestin was placed. After treatment was completed the probing depth reduced by 2-3 mm.
Treatment consisted of 2 visits.


