Ms. R.D. is a 46 years old black female, reside in Brooklyn. Patient chief complained was ‘I want my teeth clean” she does not have dental insurance and her last dental visit and radiographs are unknown. The patient uses medium manual toothbrush with Colgate toothpaste 2x a day, floss and mouth rinse are use occasionally. Her BP: first reading:161/91, second reading:152/93, pulse 73. ASA II. She is taking Amlodipine 10mg 1x per day for hypertension. The patient does not consume alcohol, smokes, or uses drugs.
EXPLANATION OF CONDITION
High blood pressure, hypertension, is a condition in which the force of the blood against the artery wall is too high. It is defined as blood pressure above 120/80 and severe if the blood pressure is above 180/100. As mentioned above the patient is taking Amlodipine (Norvac, amvaz), is used to treat high blood pressure and regulate angina ( chest pain). Amlodipine is in a family of medicines called blockers of the calcium channel. By relaxing the blood vessels, it reduces blood pressure so that the heart does not have to pump as heavily. Effects on dental treatment: Patients with Amlodipine therapy, gingival enlargement only occurs in areas where local inflammatory factors are present. Adverse reactions include light-headedness and dizziness.
HOW CONDITION IS MANAGED
HYPERTENSION: Eat healthy food, decrease salt in the diet, maintain a healthy weight, increase physical activity, manage stress, and monitor blood pressure at home.
DENTAL HYGIENE MANAGEMENT
Dental management of HTN patients: Chair position – move chair slowly. Check blood pressure prior to every visit and after treatment. Local anesthesia with a vasoconstrictor (1/100000) is permissible. Patients who are taking Beta-blockers can use Vasoconstrictor LEVONORDEFRIN.
COMPREHENSIVE ASSESSMENTS
RADIOGRAPH: FMS was taken and revealed generalized horizontal bone loss with localized areas of vertical bone loss, radiographic calculus present. No evidence of caries present.

EXTRA ORAL, INTRAORAL EXAMINATIONS
EO: Papule behind left ear. IO- Bilaterally cheek bite, exostosis on maxillary left and bilateral linea alba.
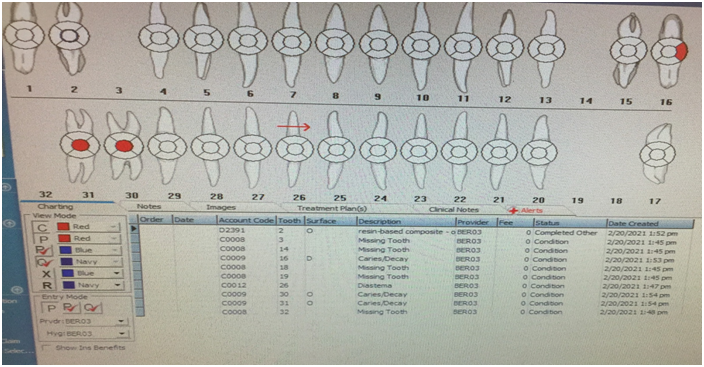
DENTAL CHARTING
Missing teeth: # 3, 14, 18, 19 and 32. Diastema tooth #26. Resin-based composite: tooth # 2-O. No clinical or radiographic evidence of caries present. Occlusion: Right side class I and Left side class II, overjet 4mm, overbite 5%.
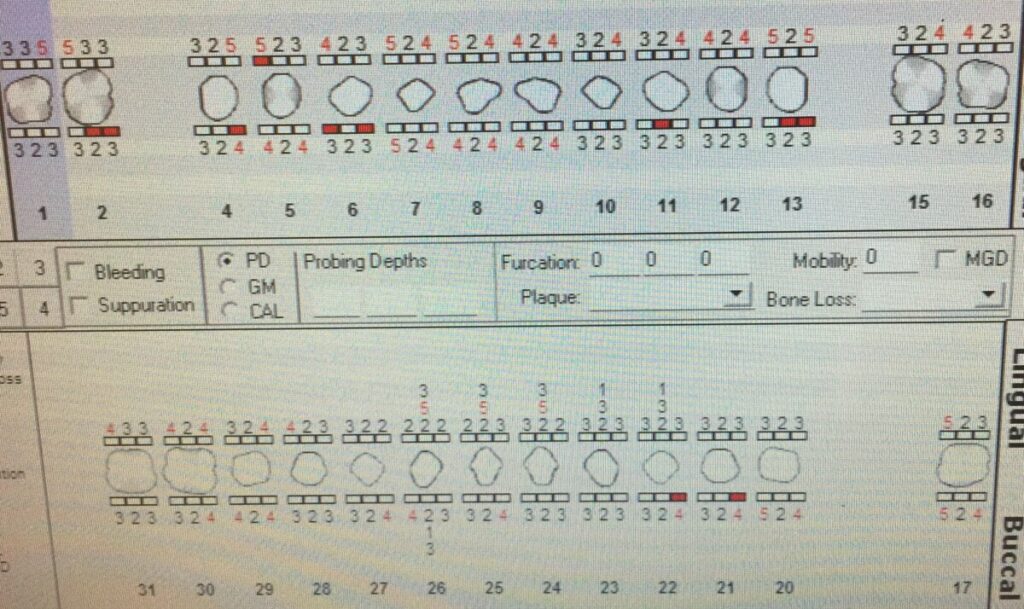
PERIODONTAL STATUS
Generalized mild gingival inflammation with rolled margins and localized bulbous papilla on lower anteriors. Localized heavy supra and sub gingival calculus on posterior interproximal and mandibular linquals region. Pocket depth ranges 2-5mm. Moderate bleeding upon probing with recessions 1-4mm and class 1I mobiity teeth #22-26.
DENTAL HYGIENE DIAGNOSIS
The patient periodontal status is: Stage III Grade B due to generalized horizontal bone loss with moderate vertical bone loss and clinical attachment loss, subgingival calculus, measurable pocket depth (2-5mm) with moderate bleeding upon probing. Recessions 1-4mm with class 1I mobility.
IMPLEMENTATION- TREATMENT –INCLUDE ALL VISIT
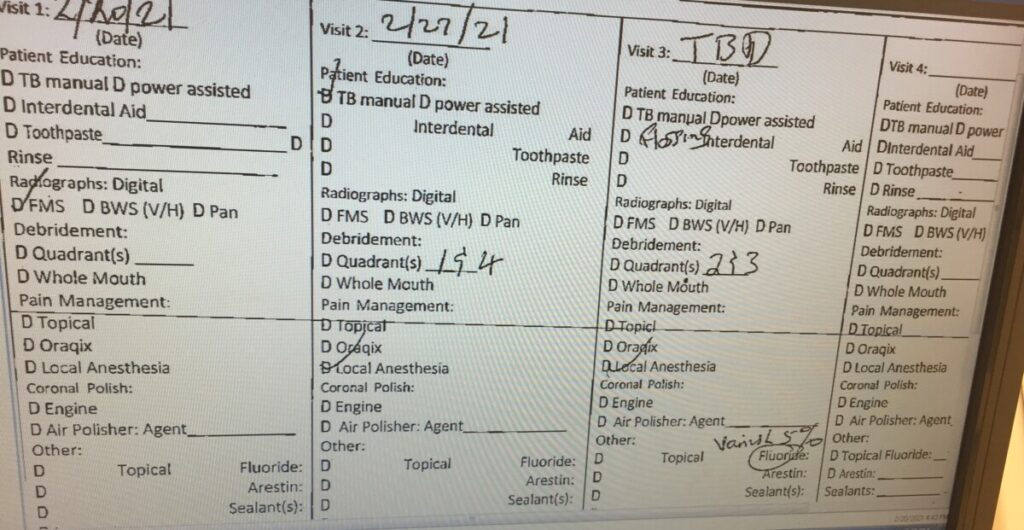
Initial visit: all assessments were completed, a treatment plan was devised, and consent was given. exposed FMS. Visit 2: PI calculated, OHI flossing taught, Scaled UR, LR quadrants using hand instruments, moderate bleeding present, used 20% benzocaine topical for any sensitivity. Visit 2: Reevaluated UR, LR quadrants, decreased redness present in previously scaled areas. PI and OHI given, hand scaled UL, LL quadrants, minor bleeding present, used 20% benzocaine topical, engine polished all four quadrants with fine paste, applied 5% sodium fluoride varnish, instructed 3 month recare.
The patient’s home care goals initially were to get her to start flossing. The majority of the biofilm present that was revealed in the plaque index was interproximal. She needed to be introduced to a routine and educated that bleeding while flossing was normal due to the inflammation she presented with and would subside with continued use of floss. On our third visit we revisited flossing and reviewed her technique. Modified bass toothbrushing was then introduced due to the marginal biofilm present on the posterior teeth. This helped to stimulate the gingiva, remove the biofilm, and reduce inflammation.
The patient reacted positively to all interventions taught and was eager to learn. The toothbrushing technique was helpful because she realized that she needs to take the time to insure all surfaces are adequately cleaned. She seemed interested in her oral hygiene as treatments progressed. She was always excited to come for the visits and always arrived early. Initially her gingiva showed more inflammation and was tender and inflamed in some areas. When all treatments were concluded there was less bleeding and firmer gingiva. There were no additional interventions developed with the patient as treatment progressed. I would not have changed any of my treatment plan. The treatment and education given to the patient proved to be efficient and helpful to the patient’s gingival health, and plaque index score.
REFLECTION
I was able to accomplish everything I planned; both educational and mechanical, for this patient. Reflecting on my clinical treatment and faculty feedback, I can conclude that a positive experience I had was the continued eagerness of my patient. She was so excited to start and gushed about the results after.
My clinical weakness was not initially checking with my 11/12 explorer for residual calculus after finishing a quadrant. I was instructed to rescale 4 areas that I finished on the next visit, but, I was disappointed that I didn’t disclose them myself. I was taught to use an even lighter touch with my explorer and it seems to be helping immensely. Also, my timing was poor, I wish I could have finish all four quadrants and assessment in two visit on a heavy case type instead of three visit.
BEFORE TREATMENT:

AFTER TREATMENT:




