The patient is a 52 year old Asian female. She is ASA II.
The patient’s medical history was reviewed and her last medical check up was in July 2023. The patient reported having high cholesterol and is taking atorvastatin 40mg once a day in the morning.The patient also reported a reduced salivary flow rate, which ists most likely due to her medication. The patient reported no other medical conditions, allergies or recent hospitalizations. The patient does not smoke or drink. The ASA classification is ASA II due to the patient having high cholesterol and is taking medication to manage it. Her blood pressure reading was 95/67mm Hg and her pulse was 85 beats per minute. The patient’s last dental hygiene service was in July 2023 in which prophy and check up radiographs were completed. Her current oral hygiene routine consists of brushing twice a day with a soft manual toothbrush. The patient reports no use of floss, oral rinses and tongue scrapers.
A comprehensive examination of the oral cavity was conducted, and I noted that the patient had exostosis, which is a benign growth of extra bone, in sextant 2 and 5. There was also generalized mild attrition with exposed dentin on maxillary and mandibular anterior teeth. Abfractions were noted on #5, 20, 21 and 28 due to excessive forces placed on teeth. The gingiva appeared red with rolled margins, puffy and leathery in consistency, and slightly bulbous interdental papilla in the anterior region. There was noticeable heavy plaque throughout the dentition with moderate bleeding on probing. The patient did not have any existing restorations.
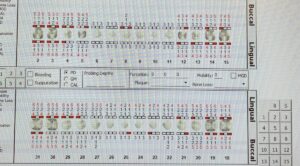
Periodontal charting was done, and the patient had 1-3mm pocket depths in the anterior region, 3-5mm pocket depths in the posterior region except for the mesial buccal aspect of tooth #15, which had a depth of 6mm. The patient also had generalized 1-2mm recession throughout the dentition which was noted (See chart).
Since the patient had recent radiographs taken in July 2023, I decided to take 4 bitewings and a panoramic radiograph due to the presence of wisdom teeth on the right side. Based on the radiographic evidence, the patient was periodontally staged at stage III, grade B due to furcation involvement class I on #19 and #30 with generalized bone loss (15-33%). Based on the radiographs, a suspicious and possible carious lesion was noted on the distal of #31, most likely due to the partial impaction of #32. Radiographic calculus also noted on the bitewings.
After the CAMBRA assessment, the patient was considered high risk due to frequent snacking, medications that reduced salivary flow resulting in xerostomia and possible caries (based on radiographs). Here is what I recommended for the patient: Biotene mouth rinse to help stimulate salivary flow, an electric toothbrush for better plaque removal, the use of floss twice daily to effectively remove trapped food debris and,lastly,an avoidance of frequent snacking as this alters the pH in the oral cavity which increase the risk of caries.
A referral was given to the patient for caries evaluation, periodontal evaluation and oral surgery.
Prior to her dental hygiene service, I used a disclosing solution to show the patient where the plaque was. Based on that, I decided to teach her both c-shaped flossing and bass brushing techniques as she had heavy plaque throughout. I made it a point to teach both flossing and brushing as they are fundamental to maintaining proper oral health. The patient was getting a full mouth scaling done and will not be returning, so I wanted to teach her the basics to implement them into her routine after the visit.
Initially I added topical anesthetic and Oraqix for pain management as part of the treatment plan due to the generalized recession. I thought the patient might be sensitive. We did not end up using any type of pain management as the patient was able to tolerate the ultrasonic and hand instruments well. I engine-polished, flossed and applied 5% fluoride varnish with instructions given.
I recommend a three month recare frequency due to her periodontal status because that is approximately the time it takes for bacteria to reproduce, affecting the teeth and gums again. Also, more frequent visits will hopefully stabilize and avoid the need for advanced treatment for periodontitis.