Case Study 1: Type II Diabetic Patient
Initial Visit: A 70 year old African American female arrives at the clinic for her dental cleaning appointment. The patient has type II diabetes and reports her most recent HbA1C was 7.0, which was measured two weeks prior to the appointment date. The patient takes Hydrochlorothiazide at 25mg daily to control hypertension, Metformin at 1000mg daily for her diabetes, and Aspirin 81 also for high blood pressure. Patient does not smoke nor drink, and has no history of allergies to anything.
The patient’s oral hygiene care at home was optimal, which includes: using an electric toothbrush 2-3 times per day, flossing using floss strings once a day, waterpik 3 times a week, and using oral rinse daily. Patient does not use a tongue scraper.
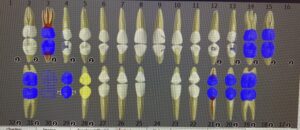
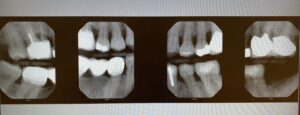
Upon extra-oral inspection, only a crepitus on the TMJ was noted. Patient reports there is no pain or discomfort. Intra-oral exam, the only notable findings were mandibular tori (nodular) and bilateral linea alba. Other findings included 6 crowns and a bridge, clinically missing third molars, missing one mandibular central incisor and two second molars. Four vertical bitewings were exposed and utilized. The radiographs showed that there was >33% of bone loss involved with localized ~30% of vertical bone loss involvement as well. There were no interproximal calculus noted, no caries, or areas of open margins.
The patient was classified as periodontitis stage III, grade C, case value: light, after all the assessments were completed. Patient education was crucial for this patient. The modified bass method was taught and I also recommended a floss threader, and articulated the use of it specifically for her bridge. Even though no referrals were given for this patient, they were advised by the professor and me to stay on top of oral hygiene care and her medications to keep the diabetes under control, since it can cause further exacerbation to her periodontal health. A full mouth cleaning was done using ultra sonic and hand instruments, and making sure to lavage the areas around her crowns and bridge. 5% Fluoride Varnish was applied towards the end with post-op instructions given. Her recall was set to 3 months in order for us to keep a track of her periodontitis and bone levels.
Case Study 2: Hypertension
Initial Visit: The patient is a 64 year old African American male. Patient reports their last dental cleaning/exam was three years ago and seeks for a proper cleaning at our clinic. Medical history shows that he does not take any medications and has no known systemic or psychological diseases. Blood pressure was measured, the first reading: 176/119 with the second reading being 165/109. The dentist on the floor was called in, but they deem that this patient needs to be dismissed and requires a medical clearance before anything can be done. The rationale was explained and referrals were given to the patient.
Second Visit: Patient came back with the medical clearance and is now taking medication prescribed by his physician. Patient has been taking Losartan at 25mg daily for his high blood pressure for three weeks. The reading during the second visit is lower than the initial visit with a reading of 137/94. Patient reports their dental oral hygiene at home: brushing once a day using a manual toothbrush, does not floss, does not use mouth rinse, and no tongue scraper.
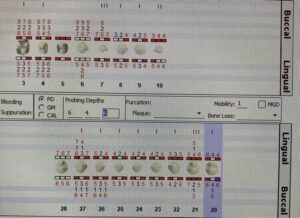
Extra-oral was within normal limits and the only notable finding for intra-oral were red patches on the labial mucosa due to possible lip biting as reported by the patient. Gingival presents with generalized severe inflammation and erythema. Interdental papilla were generalized enlarged, bulbous, and puffy. Consistency of the overall gingiva was spongy and had a shiny texture. Severe bleeding during the perio-probing.
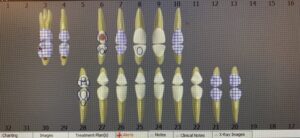
Patient had suppuration on teeth #6, #7, #21, and #28. Multiple extracted teeth, restorations, and 6 crowns were charted, caries were noted, and class I or class III tooth mobility was charted. Patient had generalized heavy build up of supra and subgingival calculus, but instructed by the dentist on the floor, only sextant five and teeth #8 and #9 can be treated. I explained to the patient why I was unable to clean or even go near the areas with suppuration, he understood. Afterwards I informed him the importance of seeing a hygienist/dentist at least twice a year in order to keep up with his oral hygiene care, as well as a medical doctor, to monitor his overall health and cardiovascular conditions. I went tooth brushing and flossing with the patient. Modified Bass and Spools method respectively. I also emphasized that to keep the teeth from becoming the same state as the ones with suppuration or class III mobility, then he must put in the time and effort to proper brush and floss daily.
The patient was classified as periodontitis stage III, grade B (without radiographic evidence), case value: heavy. I applied 5% Fluoride Varnish, but limited to the teeth without suppuration, post-op instructions were given. An adult referral was given to the patient for possible extractions on #’s 3, 4, 6, 7, 21, and 28. The adult referral was explained to the patient by the dentist and I with the rationale to all those teeth extractions. Patient understood.