Case study #1 Initial Visit
Age: 31 Ethnicity: Hispanic Sex; F
CC: “I need a cleaning.”
Medical History: BP 118/76 Pulse: 85. Controlled asthma, allergy to shrimp (symptoms include swollen mouth and throat), hyperuricemia ASA: 2
The patient informed taking Loratadine for occasional allergies, Albuterol for asthma, and Fluticasone Propionate Nasal Spray for nasal discomfort. The patient informed concern about a filling that fell off from molar #14, no pain but discomfort and sensitivity. She bought Lost Filling & Loose Cap repair to fill it.
Clinical Findings:
Extraoral/Intraoral findings: red inflamed hard palate due to maxillary partial denture. Denture stomatitis confirmed with Dr.
Gingival statement: generalized signs of severe inflammation. Localized diffuse gingiva rolling on mandibular anterior linguals. Generalized GM at CEJ mandibular teeth. Moderate BOP.
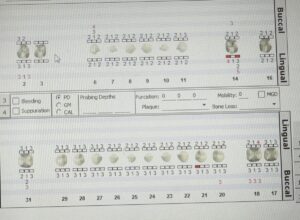
Dental Charting
Periodontal Charting
The treatment plan for this patient consisted in two appointments. During the first appointment was very important to identify the cause of the red patches on the gums, and high inflammation of the gums that the patient was suffering from. The doctor in the clinic session confirmed that the patient had denture stomatitis. I asked the patient if she was sleeping with dentures. She claimed that for a long time, she hadn’t taken off her dentures to sleep. We recommended her to stop doing that and to take off her dentures every night to sleep. The patient felt very sad and cried because she was embarrassed that her loved ones would see her without teeth. I explained to the patient the importance of removing the dentures to sleep, all the negative effects she was already suffering and the future consequences if she continued doing that. After hearing and understanding the yeast infection she was having she agreed to follow the recommendation.
Visit 1: completed all assessments. PI:2.6 poor. OHI: string floss. Introduced C-shaped flossing technique, the patient was able to properly floss anterior and posterior teeth. Referral given for caries. Ultrasonic and hand scaled Q1 and Q4 with oraqix.
Visit 2: reviewed medical history. Patient compliance with string flossing 2x/day. Introduced and demonstrated on typodont the use and benefits of electric toothbrush. Recommended Sonicare, the patient was very motivated to acquire it soon. Ultrasonic and hand scale Q2 and Q3 using oraqix. Engine polished with fine paste. Applied 5% varnish fluoride to prevent the formation of cavities on susceptible surfaces of the teeth as well as to stop the progression of caries that preexists.
Case #2 Recare
Age: 52 Ethnicity: Hispanic Sex: F
CC: “I would like and exam and cleaning”
Medical History: BP: 118/84 Pulse: 63. Hypertension Stage 1/fibromyalgia ASA:2. Patient stopped taking medication for depression as per Dr instruction (Nortriptyline) as patient feels mentally stable.
Clinical Findings:
Extraoral/Intraoral findings: moderate generalized attrition mandibular and maxillary anterior teeth. Generalized mandibular and maxillary erosion. Mild inflammation mandibular and maxillary.
Gingival statement: pink and firm gingiva non-stippled. Generalized recession 1-3mm with Class II embrasures mandibular anterior teeth. Localized 4mm pockets. Light BOP.
Dental Charting
Periodontal Charting
Initial appointment: This patient was diagnosed with hypertension (Ecuador) and fibromyalgia (New York). The patient was not taking medication for any of these conditions. In the initial appointment in 2023 she was taking medication for depression one time a day which caused her to have dry mouth. A medical clearance was required, because according to the guidelines from the American Heart Association, her blood pressure coincided with Hypertension Stage 2 (BP; 132.89 pulse; 78).
Revisit: The patient came back with the medical clearance, and I was able to continue with the treatment plan. The case value was heavy, periodontal Stage II grade B. The patient was not using dental floss, so I taught her the correct flossing technique. Ultrasonic and hand scaled Q1 and Q4 with oraqix. For dry mouth I talked about the importance of constantly drink water and I recommended xylitol gum three times a day (total of 6 pieces equal to 6g of xylitol). Referral given for caries. A nightguard was recommended to protect teeth.
Visit 2: reviewed medical history. Patient compliance with string flossing 2x/day. OHI: Modified Bass technique. This technique remove plaque in high level specially on the gingival margin. Ultrasonic and hand scale Q2 and Q3. Engine polished with fine paste. Applied 5% varnish fluoride.
The patient returned after three months for her check-up and cleaning and her case value changed from medium to light. I noticed less inflammation and light BOP. She continued flossing three times a day. I was very excited to let her know that she was doing a great job by following the recommendations and taking care of her teeth. The patient was very motivated.