Profile
- The patient is a 54 year old, Asian female.
- Middle class, resides in New Jersey with husband. The patient works in banking and has a degree in economics from a university in the Philippines. The patient has insurance and she has a dental home that is walking distance from her office.
- The patient reported she does not typically go to the dentist unless she is in pain and she reported scheduling hygiene appointments 1x/year.
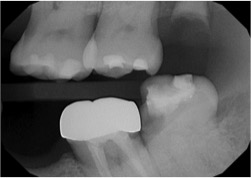
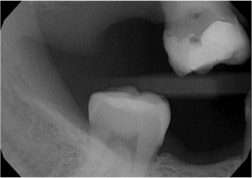
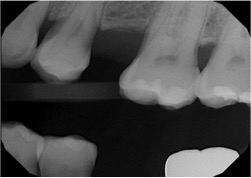
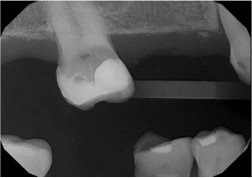
- The patient’s last dental exam, cleaning, and set of radiographs were in June 2016 and she had 4 bitewings exposed.
- She wears a partial denture on the maxillary arch, which at her initial visit she reported she did not remove at night. The patient reported she discontinued wearing her lower partial denture when it started to give her pain ~20 years ago.
- The patient reported initial work on her partial denture including extractions were completed in the Philippines about 34 years ago. The patient reported dentistry was not very advanced during that time.
- The patient reported brushing natural teeth 3x/day with a tapered end soft manual toothbrush with Colgate Total toothpaste. Patient was flossing only when food was stuck between her teeth, and using mouthwash occasionally.
- The patient presented with multiple restorations and active carious lesions.
Health History Overview
- BP: 127/74 ; Pulse: 99 ; ASA II
- The patient has been smoking 1/4 pack of cigarettes every day for 28 years and is not interested in learning about tobacco cessation.
- The patient presented with a positive history of diabetes, hypertension, and hypothyroidism.
- Diabetes onset: ~26 years ago. Pt. reports gestational Diabetes turned in to Diabetes type II when she could not lose the weight from pregnancy.
- Hypothyroidism onset from Diabetes: ~10 years ago
- Hypertension from Diabetes: ~10 years ago
- Current Medications
- Diabetes:
- Metformin 1000mg 2x/day
- Basaglar (long acting insulin) 60units 1x/day
- Humalog (rapid acting insulin) 40 units 3x/day
- Hypertension:
- Amlodipine 5mg 1x/day
- Losartan 100mg 1x/day
- Atorvastatin 200mg 1x/day
- Hypothyroidism:
- Levothyroxin 0.125mg 1x/day
- Diabetes:
Summary of Clinical Findings
- EO: Slight clicking on left side TMJ. The patient reported grinding her teeth and presented with severe attrition. IO: Erythematous lesion on the hard palate with margins where her partial denture sits. Discussed the possibility of a fungal infection due to her wearing the denture overnight. The patient presented with white, ulcerated lesions along the buccal mucosa. The patient reported unintentional cheek biting due to tight cheek contact.
- Bilateral Class I canine occlusion. No overbite or overjet as patient is missing teeth #7-10.
- Dental:
- Patient wears partial upper denture which encompasses teeth numbers 2, 4, 5, 7-10, 13.
- Class I, II, and V composite restorations on teeth numbers 3, 6, 11,14, 15, 17, 20, 21, 28, 29, 31
- Teeth numbers 1, 2, 4, 5, 7-10, 13, 19, 30, 32 missing; #16 retained root tip
- Moderate attrition on all natural teeth.
- PFM crown on tooth #18
- Deposits:
- Generalized subgingival rough/grainy calculus with clickable calculus in the mandibular posterior area.
- Moderate staining of hard tissue due to cigarette smoking and coffee consumption.
- Gingival Description and Periodontal Status
- Patient presented with an erythematous lesion on the hard palate where her partial denture sits. With my instructor, we discussed the possibility of a fungal infection due to the the patient does not remove her denture at night.
- She presented with pink gingiva that was non-stippled, rolled marginally, and soft in texture. The gingiva was flaccid around the teeth. Patient was active Periodontal type III:
- 5-6mm PD
- BOP
- Radiographic boneloss in 33% of the mouth
- Generalized 2mm recession
- Class I furcation involvement on tooth #15
- Class I mobility on teeth #11, 12, 20-28
Dental Hygiene Diagnosis
- Patient is at a high risk for caries due to multiple risk factors and behavioral indicators that contribute to caries risk.
- The patient is aware of effects of cigarette smoking on Diabetes and was not interested in tobacco cessation.
- The patient had moderate visible plaque biofilm.
- The patient presented with severe carious lesions on teeth #3, 17, 20, and a retained root tip on tooth #16. She reported she had a tooth extracted due to caries within the last 3 years.
- Radiographically, #17 is missing the mesial wall.
- Type III active periodontitis due to 5-6mm pocket depths, light BOP, radiographic evidence of boneloss, and moderate to severe recession.
Dental Hygiene Care Plan and Treatment
- Preventative Services – periodontal maintenance
- After the CAMBRA assessment, the patient was instructed to use Colgate enamel health in replacement of her current toothpaste 3x daily and to incorporate ACT anticavity mouthwash into her hygiene routine 2x daily.
- The patient was taught the use of gauze strips around teeth with no adjacent teeth for biofilm removal and the use of proxabrushes for interproximal spaces.
- Referrals were given to the patient for restoration of multiple carious lesions and periodontal evaluation. The patient was also referred to her general dentist for 1.1% NaF anticavity toothpaste.
- Subgingival air polishing was incorporated into the treatment for areas where the patient had 4+mm pocket depths and hard tissue staining.
- The patient had 5% NaF varnish applied at the end of her treatment and will have another one done at her 3 mrc.
- Debridement
- Ultrasonic: used FSI-FLI-FG 1000 & THINSERT – FIT GRIP
- This instrument allowed removal of subgingival calculus in areas the patient had 4+ mm pocket depths as well as on areas with moderate deposits.
- After removal of calculus deposits, biofilm was removed using the THINSERT for deplaquing.
- Hand Scalers: Anterior Sickle Scaler, Gracey 1& 2, 11/12, 13/14, SCNEVI 28
- Applied advanced instrumentation by using alternative instrument cutting edges, especially at the line angles of the teeth.
- Horizontal, vertical, and oblique debridement strokes were used for calculus removal.
The goal of the treatment was to remove any residual soft biofilm not removed by Ultrasonic instrumentation and to remove hard tissue staining caused by cigarette smoking.