Demographics
A 56-year-old West Indian male visited a dental office for a routine checkup.
- Prior to dental clinic visit, patient had no access to dental care due to financial hardship.
- Patient reported using a manual toothbrush and chewing on the branch from a “black sage” tree as methods utilized to care for his teeth.
Patient’s Profile/Health History Overview
- Blood Pressure: 106/75, Pulse 79
- ASA III
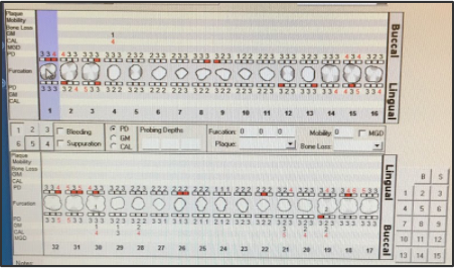
- Heavy Case Value Type / Generalized Type II with Localized Type III Perio.
- Patient last dental exam/cleaning was done in 2014. No x-ray was taken
- Health Conditions & Medications Prescribed
- Diabetes Type II
- Nateglinide 60 mg 1tab TID before meals
- Metformin HCL 500 mg 1 tab BID PO
- Cholesterol
- Pravastatin 40 mg 1tab qd PO
- GERD
- Esomeprazole 40 mg 1 cap qd PO
- Diabetes Type II
Comprehensive Assessments
Radiographs

Extraoral Examination
- Slight crepitation on right side of TMJ upon maximum opening.
Intraoral Examination
- Bilateral linea alba; coated dorsum of tongue; fissured tongue;
- Near tooth #15 has a 4mm by 3mm white patch located on the buccal mucosa;
- Near tooth #28 has a well defined 1mm white macule located on buccal mucosa.
- Patient has a low resting saliva flow-checked by chairside test and mouth mirror sticks to
- buccal mucosa.
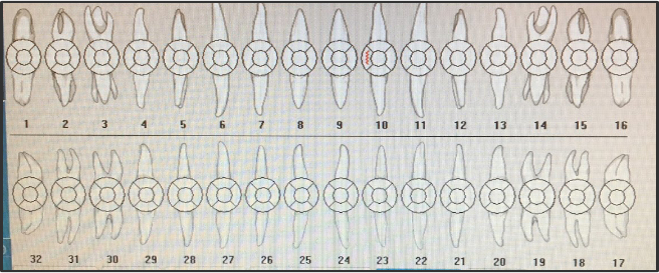
Dental Charting
- All teeth are intact with no restorations, missing, impacted or partially erupted teeth.
- Diastema between #8 and #9.
- Patient has anterior edge to edge with a crossbite between #10 and #22
- Attritions can be found between #5-8 and #21-28;
- #9 toroversion due to an accident when he was a child;
- #10 fractured on mesial.

Occlusion
- Class I occlusion with tendency to class III occlusion
Deposits
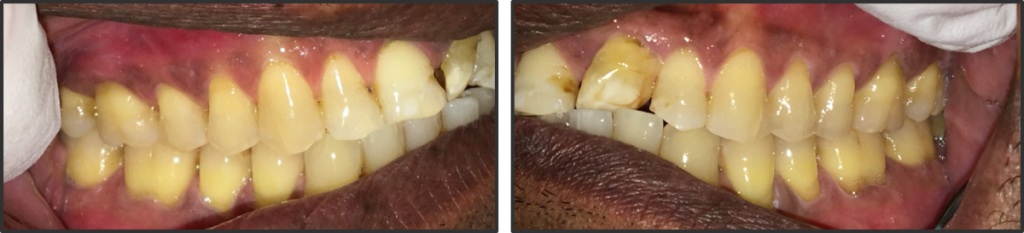
- Generalized heavy subgingival and supragingival calculus present on both arches.
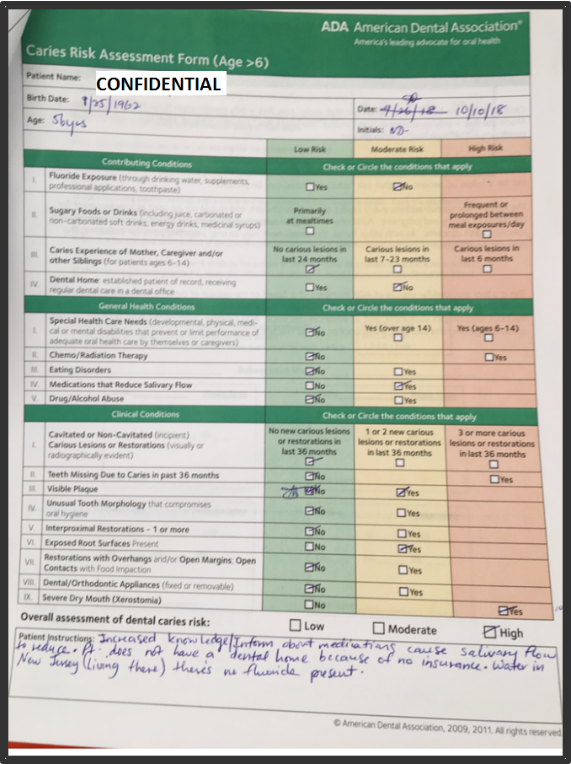
Carries Risk Assessment
- No clinical evidence of caries presented. However, patient has a high risk of caries due to:
- No fluoride exposure,
- No dental home,
- Medications that reduce salivary flow,
- Visible plaque,
- Exposed root surfaces, and
- Severe Xerostomia.
Gingival Assessment and Periodontal Status
- Gingival Description
- Generalized pink papilla with generalized melanin pigmentation, pyramidal shaped papilla, fits snugly around the teeth, firm consistency, stippling texture present and minimal to moderate BUP.
- Perio Classification
- Perio type II with localized III
- Localized Slight Periodontitis
- Generalized minimal to moderate BUP
- Generalized 2-3 mm probing depths with localized 4-6mm pocket depths
- Localized recessions on #4, #19-21, #28-30 on the buccal
- Class I and 2 furcation’s on teeth #19 and #30
- No mobility
Dental Hygiene Diagnosis
- Periodontal Diagnosis
- Type II active periodontitis due to generalized 4-6 mm pocket depths, minimal to moderate BOP, recessions and furcation.
- Grade I and 2 furcation involvements noted on buccal of #19 and #30.
- Risk for Caries Diagnosis
- Patient at high risk for caries due to multiple risk factors and minimal protective factors.
- No fluoride exposure
- Visible plaque
- No dental home
- Exposed root surfaces
- Medications that reduce salivary flow
- Severe Xerostomia
- Patient at high risk for caries due to multiple risk factors and minimal protective factors.
Dental Hygiene Care Plan
- Patient Centered Care Plan Goals
- Patient will report using Bass method toothbrush technique by 3 month recare.
- Patient will report using xylimelt by 3 month recare.
- Patient will report using hydris dentifrice (Colgate) by 3 month recare.
- Patient will report hydris mouthwash (Colgate) by next 3 month recare.
- Patient will report using the correct flossing technique by next 3 month recare.
- Patient will report using End- tufted brush by 3 month recare.
Implementation – Treatment
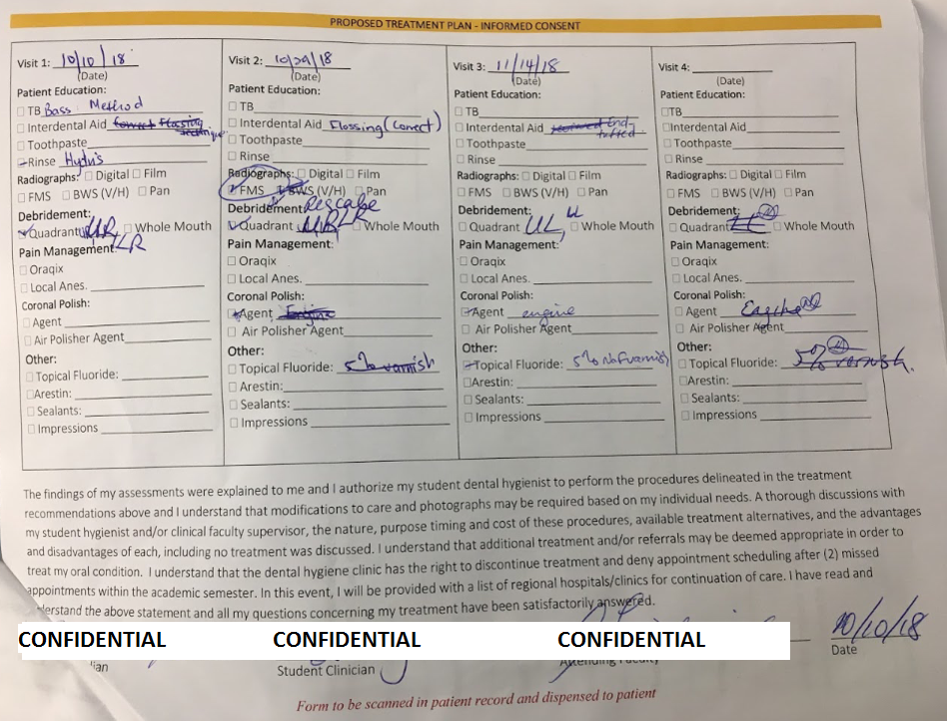
- Care Strategies/Intervention
- Bass Method Toothbrush Technique
- Correct Flossing Technique
- End-Tufted Brush
- Colgate Hydris Mouthwash
- Xylimelt
- Whole Mouth Quadrant Debridement
- Engine Polish with Fine Paste
- 5% NaF Varnish
- Preventive Services
- First Visit
- I introduced the correct method of Bass tooth brushing technique using the manual toothbrush for the first aid.
- Proceeded to educate the patient about the definition and cause of plaque, calculus and gingivitis, and how they can be removed with proper oral hygiene.
- I also informed patient that gingivitis is reversible with brushing, flossing, and rinsing.
- Second Visit
- I reviewed the Bass Method technique with patient.
- Patient informed me that he only used the method twice and after that he forgot. I did review the method with the patient and he was glad that it was demonstrated again.
- Patient advised that he uses toothpick but indicated that it was not successful in cleaning his teeth.
- Based on the findings from plaque index (0.8 Fair), patient was not effective at removing plaque around gingival margin and interproximal areas. Therefore, I introduced the unwaxed, thread-like flossing method.
- Patient requested a demonstration on how to floss. I emphasized how flossing can help reduce gingival inflammation. Patient said he will make an effort to floss before he goes to sleep. Patient was given this type of floss due to generalized embrasure type I space.
- Due to embrasure type II space on the maxillary anteriors, patient was recommended end-tufted brush.
- Due to severe xerostomia, patient was recommended to use Colgate Hydris mouthwash and dentifrice. He was requested to use these because of dry mouth; patient has a high risk of caries.
- Third Visit
- Patient was given Xylimelt – an oral-adhering discs that stick to your teeth or gums to relieve persistent dry mouth. Made with xylitol, a natural sweetener that helps stimulate saliva flow. The mild mint flavor freshens your breath and the xylitol may reduce the risk of caries.
- He was given 2 tabs on both sides of parotid salivary glands for 4 hours. Patient said that he felt the releases of the saliva in his mouth.
- First Visit
- Debridement Performed – Whole Mouth Therapy
- Patient had tenacious calculus mostly interproximal because he had not been to the dentist since 2014.
- I used the ultrasonic scaler on two to three teeth at a time starting from lingual then buccal. I managed to remove the calculus, however, there were some residual calculus interproximal and I proceeded with the hand instruments. This was done successfully throughout the debridement therapy.
- I had challenges when using the ultrasonic scaler (FSI 1000). The calculus was very tenacious to the point where I had to switch the FSI 1000 to FSI-SLI-FG 1000. So in between debridement I was using the ultrasonic scaler, explorer, and hand instruments.
- Having difficulties with removing calculus using hand instruments, I used finger assisted mesial/distal aspect advanced fulcrumming techniques especially on the lingual of maxilla.
- I also applied the opposite arch and cross arch techniques. I was able to access the difficulty areas with these advanced fulcrumming techniques very easily.
- After whole mouth quadrant (multiple visits), I used the engine polish with fine paste and applied 5% NaF varnish.
- I explained to patient that the engine polish only removes stains and plaque and not calculus.
- Patient was given important instructions after application of the 5% NaF varnish.
- Patient was advised to consume a soft, non-abrasive diet for the rest of the day, do not brush or floss for 6 hours, and refrain from hot beverages.
Continued Care Recommendations
- Patient has generalized type II perio with localized type III (Generalized 2-3 mm probing depths with localized 4-6mm pocket depths), recessions, furcation involvements, minimal to moderate bleeding upon probing, high caries risk (no dental home, no fluoride exposure, visible plaque, and severe xerostomia).
- Therefore, I recommended three month re-care interval for this patient so the hygienist can monitor, manage and remove buildup of plaque.
- To help patient maintain a good oral health, the following oral care products were being recommended:
- Correct Bass Method Technique
- Correct Thread Floss Technique
- End-Tufted Brush
- Sensodyne ProEnamel
- Colgate Hydris Mouthwash
- 5% NaF Varnish
Before Debridement

After Debridement