Demographics
G.D., Male, 29 years old, Heavy/Type 1 generalized
Assessment
Patient had nothing significant in medical history to report. Patient’s last dental exam was done two years ago. He did an FMS X-Ray and a routine cleaning.
- Patient is ASA 1
- Vital Signs: Blood pressure 122/77, Pulse 72
- Non-social drinker, non-smoker, no pre-medication needed, no current medications, no systemic conditions present.
Oral Pathology
No significant findings on the intraoral examinations.
Dentition
Bilateral Class 1 Occlusion.
- Patient has edge to edge bite on the right side, #4 and # 29 has cross bite, 2mm overjet and 10% overbite on the left side of #10 and #23.
- Attrition on #2, #5, #6 and #19 due to patient grinding.
- Abrasion on #29-31, #18, #4 and #20 shows beginning of demineralization.
- Patient is missing #1, #16, #17 and #32.
- Patient has composite restorations on all posterior teeth on both arches.
- No tooth anomalies or active caries present.
Periodontal
Case Type 1 Generalized
- Generalized 1-3 mm probing depths with localized 4-5mm especially molar regions
- Generalized moderate bleeding upon probing on all surfaces
- Localized recessions on #3 and #24-25 lingual
Generalized normal melanin pigmentation with localized gingival inflammation on #3 mesial related to poor crown contour, gingiva around #19 crown is bulbous.
Oral Hygiene
Patient’s initial plaque score was 1-Fair. Revisit plaque score was 1-Fair. Heavy case value patient with generalized supra and sub gingival calculus. Calculus was more prominent on mandibular anterior facial and lingual on #22-#27
Planned OHI: On the patient’s first visit of the examination (disclosing), patient advised he brushed his teeth twice daily. Upon findings with plaque index, patient was not effective at removing plaque around the gingival margin and interproximal areas. I therefore introduced correct method of Modified Bass tooth brushing technique using the manual toothbrush for the first aid. I went on to educate the patient about the definition and cause of plaque, calculus and gingivitis, and how they can be removed with proper oral hygiene.
On the patient’s second visit, I did the plaque index; score was 1-Fair. Patient stated that he was able to implement his toothbrush technique only one time during the first prevention. He said he forgot how to do it after the first day. I reviewed the Modified Bass tooth brushing technique with patient again and taught the next aid of proper flossing method since most plaque retention was noted in interproximal areas. Patient stated that he does not floss at all because it was time consuming. Patient’s gingiva, however, showed no redness and no post op discomfort from previous visit.
I emphasized how flossing can help reduce gingival inflammation. I began our conversation by instructing the proper way of flossing: choose right middle finger to hold floss, and excess onto left middle finger of left hand, slide in a short sawing motion, make c-shape against the tooth and use up or down movement. I also recommended that the patient make additional attempts to floss more frequently. Preferably, he should floss once a day, especially at night before he goes to sleep.
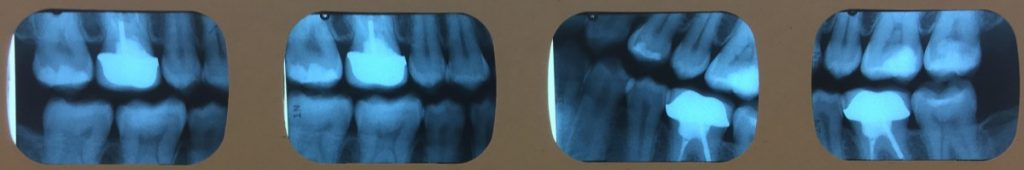
Radiographs
Patient had FMS x-ray done 2 years ago. Patient required 4 bitewing radiographs to confirm periodontal conditions.
Treatment Management
Visit 1
I reviewed patient’s medical history and intraoral examination were within normal limits. Completion of probing and calculus detection were done.
Visit 2
I reviewed his medical history and intraoral examination again- within normal limits.
Plaque score was 1(Fair). Introduced correct method of modified bass tooth brushing technique, applied 20% Benzocaine topical and scaled LR quadrant with hand instruments.
Visit 3
Plaque score was 1(Fair). Introduced the second aid of flossing, re-scaled LR quadrant for residual calculus with hand instruments, applied 20% Benzocaine topical and scaled UR quadrant with hand instruments.
Visit 4
Plaque score was 0.5 (Good). OHI- reviewed flossing with patient, re-scaled LR and UR quadrants, applied 20% Benzocaine topical and scaled UL and LL quadrants with hand instruments, engine polished and applied neutral sodium fluoride gel for 4 minutes (NaF 2%).
No medical, social, psychological factors were present that impacted treatment.
Based on the plaque scores, I would not change any part of my treatment plan or the patient’s education plan. Patient’s plaque score was taken three times throughout the treatment plan; the first and second scores were 1 and the final score during visit 4 had reduced to 0.5 (Good).
I showed the patient the difference in scores and complimented him of his oral hygiene practice. I told him to continue following the instructions provided for tooth brushing and flossing.
Evaluation
Initially, the patient did not show any interest in his oral hygiene. However, as treatment progressed, I showed him where the plaque retention in his mouth was located and visible using the disclosing solution. Patient became more inclined and interested in my demonstration and instructions.
The patient’s gingiva at the initial appointment was a generalized healthy normal melanin pigmentation with localized gingival inflammation on #3 mesial related to poor crown contour, gingiva around #19 crown is bulbous and fits snug around the tooth with localized recession.
No additional interventions were developed. I only recommended the Modified Bass tooth brush and flossing method because they were the best tools for the patient. Patient was willing to learn since his plaque score had reduced and he was motivated by that.
Reflection
I believe I accomplished everything I planned because my patient’s plaque score was reduced. My patient was motivated by the methods I thought and demonstrated. Introducing the modified bass tooth-brushing and flossing method were important for the patient’s education. Overall, I was very satisfied because I was able to motivate my patient to conduct health oral hygiene practices.


