Patient profile:
Ms. M is a 35 y.o. Caucasian female presented for a dental cleaning. She is non-smoker, reports no alcohol or drug use, and has allergie to pollen. Patient states she uses a manual toothbrush 2x/day, toothpaste Colgate, flosses 2x/day.
Chief complaint: “I need a dental cleaning and I have sensitive areas on upper back side”.
Vitals: BP: 101/74 corresponding to normal, P: 87, ASA-2.
Med/dental Hx: Reports no hospitalizations in the last 5years. No allergies. No taking any Medications. Her last dental checkup with cleaning was a 3 year ago.
Clinical Findings:
Extraoral/Intraoral findings: Both side TMJ clicking sound. Palatal Tori, slight Linea Alba present.
Occlusion: molar relation Class I bilateral. Overjet- 3mm. Overbite- 30%. Localized attrition on anterior incisors. Diastema on front teeth.
Gingival statement: Generalized pale pink color of the gingiva, fits enlarged around the teeth, interdental space is filled with pyramidal shape bulbous papilla, rolled gingival margin, soft consistency, and smooth texture.
Dental Charting:
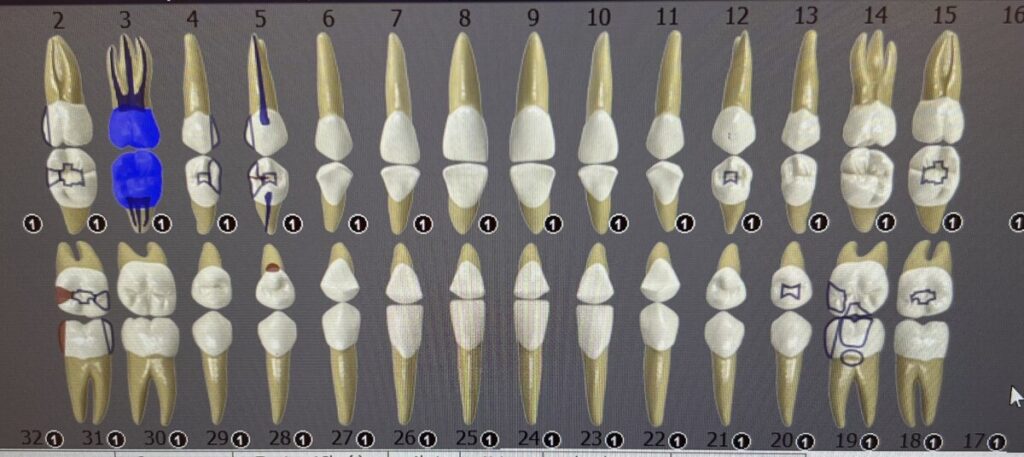
- Composite restorations: #2-DO, #4-MO, #5-DO, #12 -O, #15-O, #18-O, #19-OMB, #31-OM.
- Inlay on #5-O and 18-DO.
- Root Canal : #3, #5.
- Porcelan Crown #3.
- Possible Caries lesions: #31-D, #28-L.
Periodontal Charting:
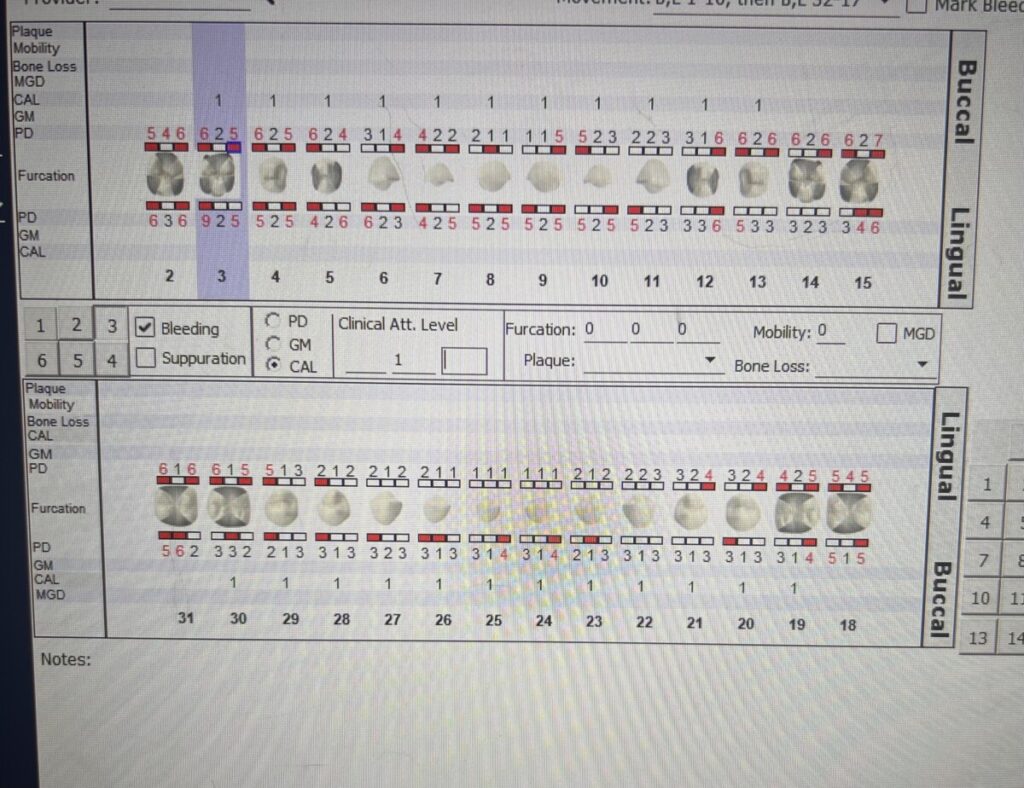
Generalized heavy bleeding on probing. Probing depth ranges between 1-6 mm on anterior teeth and 3-7 mm on posterior teeth, with maximum probing depth 9 mm on #3-DL.
Generalized gingival recession of 1 mm
During the patient’s initial visit, a comprehensive examination of the oral cavity was conducted, revealing localized attrition. Patient required FMX radiographs for evaluation of carious lesions and any bone loss since she has not had it in about 3 years. A Full Mouth Series was performed, which revealed a Heavy Stage III Grade B case value, due to the presence of generalized radiographic evidence of calculus, generalized more than 15% RBL, localized 30-50% RBL on the first molars. These findings underscored a notable presence of periodontal disease, prompting immediate attention to safeguard the patient’s oral and systemic well-being. Developing a comprehensive treatment strategy was crucial to address the patient’s concerns and prevent any deterioration in their oral health.

Periodontal Diagnosis: Periodontitis Stage III/Grade B (with radiographic evidence). Caries risk– High, due to active caries lesions. Case value–Heavy (due to heavy interproximal calculus).
Dental Hygiene Care Plan:
The patient returned for an additional 5 visits to complete her treatment plan.
Visit 1: All assessments completed included CAMBRA, recommended establish regular cleaning and use Xylitol gum 2-3 times per day for carries prevention. FMS exposed. The patient has been recommended to visit a dentist for an evaluation focusing on the presence of possible cavities.
Visit 2: Reviewed MH, DH. PI/OHI-based on PI score (1.66-Fair), a significant accumulation of plaque was noted on the tooth surfaces, prompting the introduction of the Modified Stillman’s toothbrushing method, specifically tailored to address the patient’s gingival recession. Applied Oraqix (2.5%/2.5% lidocaine/prilocaine) for pain management. Ultrasonic and hand scaled Q1.
Visit 3: Reviewed MH, DH. Tissue re-eval, PI/OHI- based on PI score (1.5-Fair),
A notable amount of plaque was observed in the intraproximal areas, prompting the introduction of the C-shaped flossing method to effectively address and remove plaque from these regions. Applied Oraqix (2.5%/2.5% lidocaine/prilocaine) for pain management. Ultrasonic and hand scaled Q4.
Visit 4: Reviewed MH, DH. Tissue re-eval, PI/OHI- based on PI score (1.0-Fair),
a tongue scraper was introduced to address specific concerns related to oral hygiene and overall mouth cleanliness. Appled Oraqix (2.5%/2.5% lidocaine/prilocaine) for pain management. Ultrasonic and hand scaled Q3. Arestin Placement has been recommended for sites with pocket depths measuring 5mm on tooth #31ML, #30DL, #30ML, and #29DL.
Visit 5: Reviewed MH, DH. Tissue re-eval, PI/OHI- based on PI score (0.9-Fair), Proxy brushes have been recommended for cleaning the interproximal spaces of the anterior incisors. Applied Oraqix (2.5%/2.5% lidocaine/prilocaine) for pain management. Ultrasonic and hand scaled Q2. Engine Polished with fine toothpaste. The application of 5% fluoride varnish was performed to enhance enamel strength, prevent decay, and promote overall oral health.
Continued Care Recommendation: An 8-week reevaluation of Arestin has been scheduled, and a 3-month re-care interval has been recommended for the patient due to the diagnosis of periodontitis, significant subgingival and supragingival calculus buildup.
During the limited focus visit, there was notable improvement in the patient’s probing depths:
The probing depth decreased from:
- 5 mm to 4 mm on #31ML,
- 5 mm to 4 mm on #30DL,
- 5 mm to 3 mm on #30ML,
- 5 mm to 2 mm on #29DL.
Periodontal Charting:
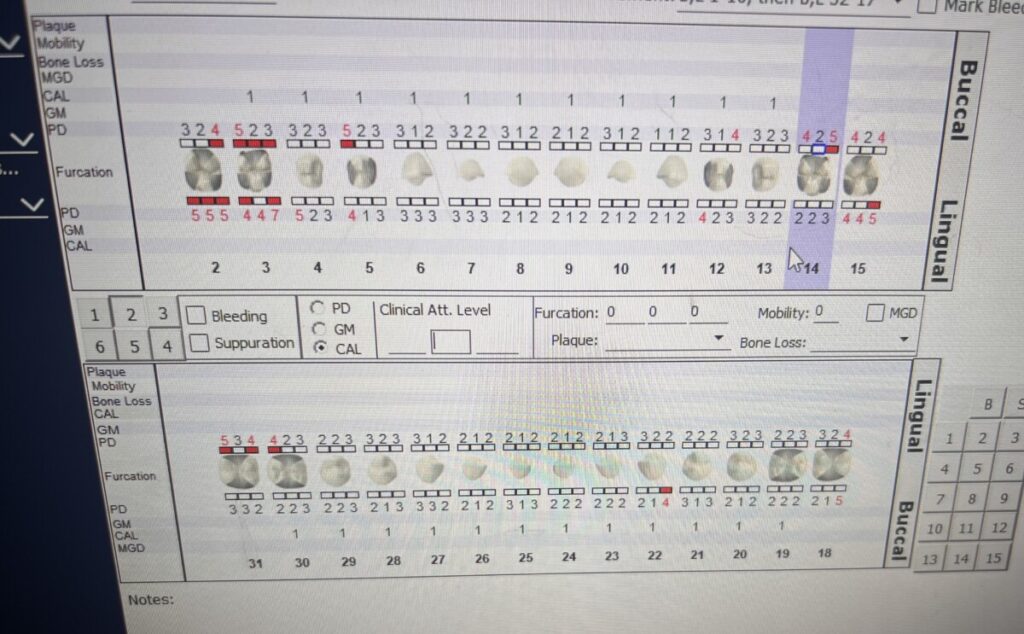
The patient expressed satisfaction and appreciation for the rapid and minimally invasive procedure, which led to significant enhancements in their oral health. Through diligent monitoring of the patient’s progress and providing attentive follow-up care, I ensured the delivery of exceptional service and maintained the ongoing health of the patient’s oral cavity.


