CASE STUDY #1
Patient Profile
- 60 year old Caucasian female
Vital Signs
- Blood Pressure: 145/95
- Pulse: 93
- ASA: III
Medical History
- Type II Diabetes. Presented in clinic with A1C level of 8%. Patient had a follow up appointment scheduled two weeks later to have A1C level re-examined.
- Current medication(s):
- Metformin 2000mg daily: (2)500mg in the morning and (2)500mg tablets in the evening)
- Daily multivitamin
- Allergies: Penicillin
- Smoking: Pack-a-day smoker for 40+ years
- No recreational alcohol or drug use
- Dental history:
- Minimal over the last ten years. Patient does not have dental coverage and only goes to the dentist when absolutely necessary
Assessments
- EO/IO
- Fibrotic nodules noted on thyroid – patient is aware and followed up with a thyroid specialist for a biopsy (results were negative; benign)
- Dental
- Patient presented with multiple missing teeth, a loose bridge and receding margins on most restorative crowns. Class II malocclusion (on left side; could not determine right side due to missing teeth #1-5) with 50% overbite and 6mm overjet. Attrition #22-26.
- Class II Mobility was noted on several teeth
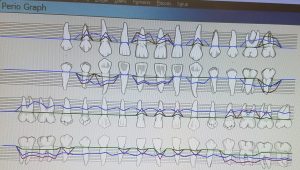
- Gingival/Perio
- Patient presented with moderately inflamed gingival tissue that appeared pink, bulbous, blunted and flaccid.
- Generalized Type III, Localized Type IV Periodontitis was present with 3mm-5mm probing depths with localized 6-7mm probing depths, confirmed with the exposure of a Full Mouth Series.
- 8 sited of Arestin were placed on this patient in Fall 2017 and re-evaluated in Spring 2018 (a 1mm improvement was noted on 5 out of the 8 sites).
- Patient presented with moderately inflamed gingival tissue that appeared pink, bulbous, blunted and flaccid.
- Calculus Detection
- Heavy subgingival calculus deposits were noted throughout the patient’s dentition.
- Radiographs
- A Full Mouth Series was exposed in Fall 2017 and utilized during all clinic sessions
Implementation
- Patient was extremely sensitive to the ultrasonic and due to increased A1C level, the Doctor on the clinic floor approved selective hand scaling. Therefore all scaling was performed with hand instrumentation. The ultrasonic was used to debride the tissue after scaling was completed with 20% Benzocaine topical for pain management.
- Referrals were given for: Dental examination, Periodontist and Oral Surgeon for multiple findings during my intraoral examination and evidence from the Full Mouth Series.
Evaluation
- Patient was placed on 3-month recalls. She was first seen in Fall of 2017 (complete S & RP with 8 sites of Arestin placed) and returned for her 3-month recall in Spring 2018 and to re-evaluate all 8 Arestin sites.
- As of her Spring 2018 appointment, she has yet to follow up on all her referrals.
PEDO PATIENT
Patient Profile
- 8 year old female patient presented in the clinic for a cleaning.
Medical History
- Review of medical history revealed no medical concerns, allergies or hospitalizations; overall, she was a healthy child.
Assessments
- The patient presented with two missing primary teeth, no evidence of caries and minimal calculus.
Implementation
- We counted her teeth together as I charted her current primary and permanent dentition present. I performed a PI index, used a Gracey 1/2 scaler to remove any calculus present and completed the cleaning with a rubber cup polish using fine paste.
Evaluation
- No referrals were given, and the patient was placed on a 6-month recall.
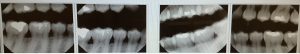
STAIN REMOVAL
Patient presented with significant extrinsic staining. I used hand scaling and the the ultrasonic to remove the present staining. Below is a picture of the maxillary arch, lingual surfaces, with the UR quadrant staining removed and the UL quadrant present staining as a comparison.
CASE STUDY #2
Patient Profile
- 43 year old Hispanic female
Vital Signs
- Blood Pressure: 128/82
- Pulse: 82
- ASA: I
Medical History
- Healthy
- Current medication(s):
- Daily supplements which include: blessed thistle (rosehips), paw paw, and chamomile
- Allergies: No allergies
- Non-smoker
- No recreational alcohol or drug use
- Dental history:
- Patient was last at the dentist in February 2016.
Assessments
- EO/IO
- Patient presented with prominent maxillary and bi-lateral mandibular tori. On patients second (and last) visit, she presented with multiple minor ulcers on her maxillary tori.
- Dental
- All teeth present (including third molars). Class I occlusion with 10% overbite and 2mm overjet. Abrasion noted on all premolars with attrition on all mandibular anterior teeth.
- Gingival/Perio
- Patient presented with pink, firm, tapered and stippled gingiva. Generalized 1-3mm probing depths with localized 4-5mm probing depths. Type II Periodontitis, with generalized horizontal bone loss, confirmed by digital bitewings.
- Calculus Detection
- Heavy subgingival calculus deposits were noted throughout the patient’s dentition.
- Radiographs
- 4 Horizontal bitewings were exposed on her last visit (May 11th, 2018) and utilized during the clinic session.
Implementation
- Patient is extremely sensitive due to generalized recession so 20% Benzocaine topical and Oraqix was used for pain management. I was able to utilize the ultrasonic and hand scaling during treatment and finished with a coarse prophy paste. Patient refused fluoride treatment.
Evaluation
- Patient was placed on 3-month recalls.