Assessment: A 26 years old, Caucasian female patient visited to get a dental cleaning. Blood pressure was taken – 107/65, corresponds to normal. First, reviewed the patient’s medical, social, dental history through patient interview. Patient reported she has no seasonal allergies and no hospitalization or surgeries in the past 5 years. Patient does not take any medications. Patient reported she smokes tobacco through a vape and also marijuana everyday. ASA: 2 due to smoking. Patient stated that her last physical was 2 years ago. Patient stated last dental visit was in July 2021 for a coronectomy and 1 PA was taken. Last dental hygiene services were done about 5 years ago. Patient stated that ortho treatment(braces) was done as a teenager but currently does not wear her retainers. Patient stated that her gums bleed when she brushes. Patient reported she uses manual soft TB, Colgate toothpaste, brushes twice a day. Patient reported that she flosses twice a week and rinses with Listerine oral rinse occasionally. Patient reported he does not use a tongue cleaner.
An Objective finding was proceeded. During the extraoral and intraoral examination, Nicotine stomatitis present. Bilateral linea alba present. On labial mucosa between #23 and #26, small, black, scattered remnants of tattoo present.
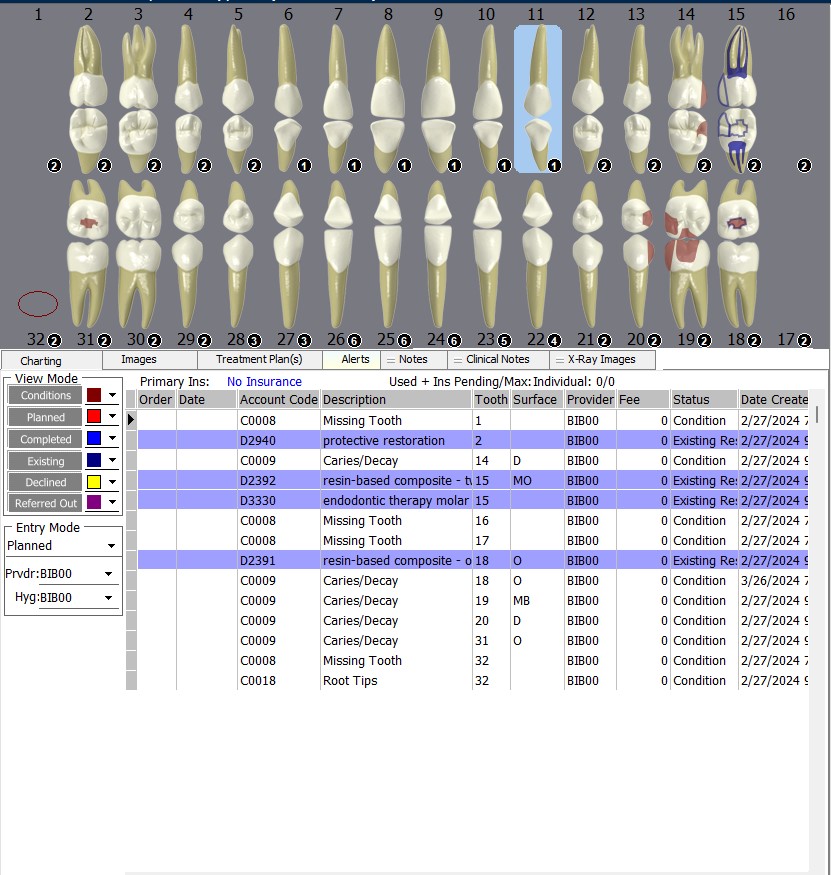
Dental chart recorded and patient had class I occlusion on right side and class II, division II on left side, overjet 7mm, overbite 10%. Also, Patient had generalized attrition on all anteriors. Gingival statement was generalized red, enlarged, retractable, friable, rolled, gingiva with localized bulbous gingiva on lower anterior linguals. (Pt is a smoker, right-handed – appearance of gingival tissue on the right side reflects effects of smoking, more redness, puffiness, rolled, shiny).
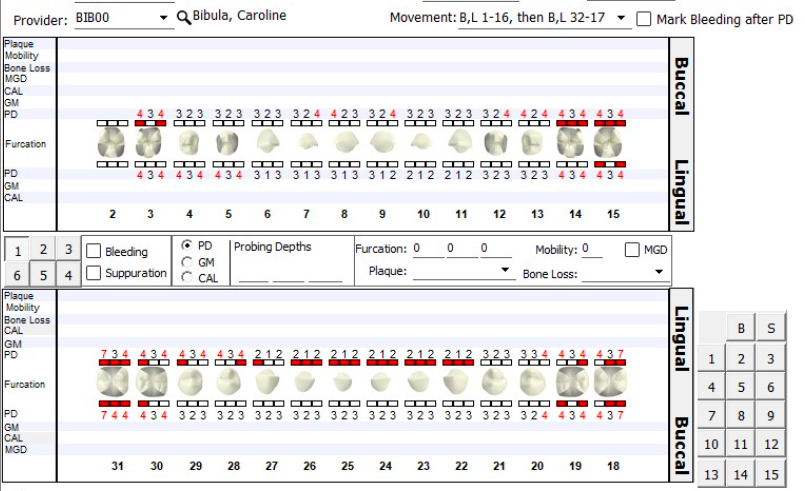
Perio charting was recorded. Generalized 1-3mm PD with localized 4 mm PD on some posterior teeth. Localized 7 mm PD present on the distal of mandibular 2nd molars. Heavy BOP. No mobility was detected. Calculus was generalized supra and subgingival calculus – case type decided as heavy. Stain was moderate.
Diagnosis: With radiographic evidence, perio status was diagnosed as generalized severe gingivitis. Caries risk was high/ CAMBRA done – recommended patient to use Listerine total care for additional fluoride exposure. Advised patient to be more proactive in receiving regular dental care. Advised patient to eat more fruits and less frequent snacking on candy.

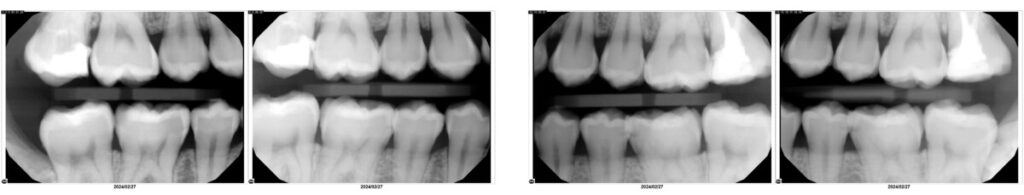
Since the patient underwent x-rays a few years ago and now exhibits localized pockets measuring between 4-7mm, I explained to her the necessity of taking x-rays. Additionally, the patient mentioned having undergone a coronectomy on one wisdom tooth while the others have yet to be removed. The patient approved for taking 4HBWs and a PAN. Radiographic findings were suspected recurrent decay on #14-D. Carious lesions present on #19-M and #20-D. Suspected incipient caries present on #12-D, #13-M, #29-D, and #30-M. Calculus present. Tooth #1 and #16 unerupted. Tooth #17 unerupted and impacted. Tooth #32 retained root tips (post-coronectomy). No jawbone abnormalities present. Tooth #15 has RCT with MO filling.
Plan: Completed all intake data/ assessment. Tx plan developed and discussed with patient and patient signed the consent. Exposed 4 HBWs and panoramic x-rays. Radiographic findings were discussed with the patient and a copy of x-rays were provided to patient. Patent signed radiology release form. Discussed clinical findings and diagnosis of gingivitis with patient.
Detailed Tx plan was:
- Visit 1 – complete assessments, discuss CAMBRA, expose radiographs, discuss diagnosis, introduced OHI – modified bass technique.
- Visit 2 – Re-eval, PI/OHI – review modified bass technique/introduce flossing, apply topical benzocaine 20% and administer LA (as needed), scale Q1 and Q4.
- Visit 3 – Re-eval, PI/OHI – review flossing/introduce tongue scraper, apply topical benzocaine 20% and administer LA (as needed), scale Q2 and Q4, engine polish with coarse prophy paste, apply 5% sodium fluoride varnish.
Implementation:
- Visit 1 – Vital signs were taken, and a BP of 107/65 and PR of 67 recorded. Medical and dental history taken and discussed. ASA II was designated based on current smoker. All assessments completed. Digital radiographs were exposed, and findings were reviewed with patient and a copy of the X-rays was provided on a USB drive. Completed CAMBRA assessment to obtain caries risk and provided appropriate recommendations. Oral hygiene instructions were given – The patient was shown the modified bass technique, and they were able to replicate the technique. Referral to General Dentist, Oral surgeon, and Primary Physician was given.
- Visit 2 – No change in medical history, no recent hospitalizations or surgeries. Reevaluation of patient completed. The patient stated she incorporated the modified bass technique and started brushing twice a day. Diagnostic intraoral pictures were taken to capture supragingival calculus located on the lingual surfaces of the mandibular anterior region. The patient reports she was not able to follow up on the referral given, due to no insurance. A list of dental clinics was given to the patient. PI acquired – 1.9 (Poor). Oral hygiene instructions were given – The patient was shown how to floss properly, and they were able to replicate the technique. The patient denied Local Anesthesia. Topical Benzocaine 20% and Oraqix (Lidocaine 2.5% and Prilocaine 2.5%) was applied. Q1 and Q4 were scaled with hand and ultrasonic instrumentation. Instructed patient to rinse with warm salt water if any discomfort; avoid spicy/peppery and acidic food); tomorrow continue with OHI given.
- Visit 3 – Re-evaluation completed. Patient states she started flossing 5x a week. Previously treated areas show decreased inflammation and the gingiva is less red, enlarged, retractable, rolled, and bulbous. A new PI score acquired – 1.9 (Poor), improvement since previous visit. The use of a tongue scraper was taught to the patient, and the patient demonstrated it successfully. The patient denied Local Anesthesia. Topical Benzocaine 20% and Oraqix (Lidocaine 2.5% and Prilocaine 2.5%) was applied. Scaled Q2 and Q3 and residual calculus from Q 1 and Q4 with ultrasonics and hand instrumentation. Engine polishing completed with coarse prophy paste. 5% Sodium fluoride varnish was applied, and post op instructions were given. Instructed patient to rinse with warm salt water if any discomfort; avoid spicy/peppery and acidic food); tomorrow continue with OHI given. Recare recommendations given and recare appointment/interval set at six months.
Evaluate: All 3 visits contained a two-week gap. Patient had heavy supra and subgingival calculus. I used cavitron to remove a significant amount of heavy calculus that was confined to the teeth. I also hand scaled and used gracey’s in order to remove subgingival calculus. As a result of evaluating the patient’s gingiva after 2 weeks, a notable change was observed.
Continued Care Recommendations: Recare appointment/interval set at six months due to generalized gingivitis. Stressed the importance of following up on referrals given for suspected caries and to evaluate 3rd molars. Reviewed with the patient the significance of routine dental cleanings and maintaining proper oral hygiene at home to uphold optimal oral health. This will help in preserving healthy teeth and gums, by minimizing the chances of gum disease and carious lesions in the future.



The initial image displays the mandibular anterior lingual surfaces with substantial supragingival calculus confined to the teeth. The subsequent images, captured four weeks post-cleaning, illustrate significant improvements. In the third photo, noticeable changes include a shift to pink interdental gingiva and the absence of bulbous gums. The patient was very satisfied with her results.
Document: All intake data/ assessment documented. Patient signed all documents and consent. Referral letter was given for evaluating suspicious caries and impacted wisdom teeth.
***The patient consented to the taking and sharing of pictures.


