Initial Visit:
A 65-year-old Caucasian female (she/her) presented to the clinic for dental cleaning with normal vitals. Upon medical history review, the patient reported having her thyroid removed due to thyroid cancer and taking prescription Synthroid 112mg per os daily as prescribed by her physician. I asked the patient if she was experiencing xerostomia, which I know to be a common oral issue seen in patients with no thyroid or hypothyroidism. The patient replied “No.” The patient also reported being allergic to Floxin, a medication used to treat ear infections in the past. According to ASA guidelines, I classified her as ASA 2.
Extraoral examination revealed asymptomatic clicking on the right TMJ and no thyroid felt upon palpation. Intraoral examination revealed an amalgam tattoo on the left ventral surface of the tongue, adjacent to tooth #19-lingual, a high vaulted palate, and a fissured tongue. Saliva production from all salivary glands was normal, ruling out Xerostomia. The patient’s gingiva was bulbous and inflamed along the lower anterior teeth, with localized puffy, spongy tissue around tooth #12. Suspicious caries lesions were detected on teeth #8 mesial-lingual and #15 occlusal. Heavy supragingival calculus deposits were seen on the lingual surfaces of the lower anterior teeth, with attrition on the incisal edges.
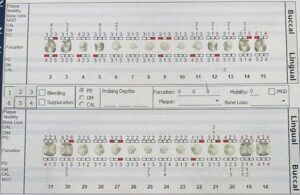
The periodontal assessment revealed several >3mm pocket readings with bleeding upon probing. One 8mm probing depth with exudate on #12 distal-lingual was present. A doctor was called to access the pocket and determined it safe to continue with assessments and treatment, and authorized an FMS to be taken.
I determined the patient’s case value heavy, caries risk severe, and periodontal status Stage II Grade B (pending radiographs). Due to the heavy calculus deposits, I created a treatment plan with two visits, to ensure enough time to effectively remove all calculus deposits. I disclosed the patient and recorded the Plaque Index score. The P.I. score was 2, corresponding to poor, with plaque mainly interproximal. Therefore, I taught the patient how to use the Listerine access flosser, to make flossing easier and more efficient for an older patient like herself with limited dexterity. I began scaling the right side of the mouth, with a plan to scale the left side on visit 2. After I completed scaling the left side of the mouth, a referral was written for evaluation of the deep periodontal pocket and caries lesions detected during the visit. The patient was dismissed.
Visit 2:
I reviewed the medical history and evaluated areas scaled from the previous visit. I inquired if the patient incorporated the Listerine access flosser introduced in the previous visit, to which the patient replied “No.” However, the patient reported that the areas previously scaled bled less while brushing. This was important for me to know because patients with no thyroid may suffer from delayed healing. Also, the patient also reported that she began to feel sensitivity to cold in the front lower right teeth after the cleaning, but it subsided gradually. I informed the patient that calculus was on the root of the teeth and that when removed the tooth will be exposed, leading to sensitivity. I reassured her that this is common when removing calculus from teeth with root exposure, and briefly advised her to continue the use of Sensodyne toothpaste to help with the sensitivity to cold.
I exposed an FMS, which showed a localized vertical defect on tooth #12-distal and generalized 15-33% horizontal radiographic bone loss. The caries lesions detected clinically were not seen on the radiographs. The radiographs supported my assessment of her periodontal status being Stage II Grade B Periodontitis.
After informing the patient of all findings, I taught the patient power toothbrushing, emphasizing the benefits of using the power toothbrush over a manual toothbrush with limited dexterity. I finished the right side of the mouth, scaled all residual calculus on the left side, and applied 5% sodium fluoride varnish to help with the sensitivity reported earlier by the patient. The patient was extremely satisfied with the level of care she received. The patient was dismissed with post-op instructions for the fluoride varnish, a copy of her radiographs, and a smile from ear to ear.