CASE STUDY #1
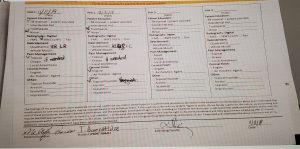
Mrs. B.N. is a 65 years old Indian female. The middle class lives with her husband in Brooklyn. She did not have dental insurance and visits our clinic regularly. Her last visit, for cleaning to our clinic was March 2019. The patient uses a manual toothbrush and Colgate toothpaste 2x a day, flossing 1x a day. The patient does not use oral rinses and tongue cleaner. The patient came to the clinic for regular recall cleaning. The BP: first reading:151/87, pulse 85, Last reading:150/88, pulse 84. ASAII. The patient does not consume alcohol, smokes, or uses drugs. She is taking Valsartan 320mg, Atorvastatin 20mg, and Aspirin 81mg. medications are for high blood pressure and cholesterol.
Explanation of Condition
High blood pressure, hypertension, is a condition in which the force of the blood against the artery wall is too high. It is defined as blood pressure above 120/80 and severe if the blood pressure is above 180/100. One of the risk factors developing hypertension is high cholesterol which is fatty deposits in blood vessels. The body needs cholesterol to build healthy cells but high levels of cholesterol can increase the risk of heart disease and hypertension.
HOW CONDITION IS MANAGED
HYPERTENSION: Eat healthy food, decrease salt in the diet, maintain a healthy weight, increase physical activity, manage stress, and monitor blood pressure at home.
HIGH CHOLESTEROL: Take the medicine as directed, make healthy lifestyle changes, use foods lower in saturated and trans fats, and maintaining a healthy weight. Check cholesterol levels regularly. If do not have heart disease every 4 to 6 years.
DENTAL HYGIENE MANAGEMENT
Dental management of HTN patients: Chair position – move chair slowly. Check blood pressure prior to every visit and after treatment Local anesthesia with a vasoconstrictor (1/100000) is permissible. Patients who are taking Beta-blockers can use Vasoconstrictor LEVONORDEFRIN.
COMPREHENSIVE ASSESSMENTS
RADIOGRAPH: To take an X-ray on the left side was difficult due to the multinodular palatal torus located on the left side from the midline of the palate. Localized bone loss most posterior region, no evidence of caries present.
SUMMARY OF CLINICAL FINDINGS
EXTRA ORAL, INTRAORAL EXAMINATIONS
EO- WNL. Multiple macules on the face. IO- Fordyce granules, bilateral linea alba, multinodular palatal tori located left side from the midline of the hard palate. White- bluish hyperkeratotic lesion on the anterior 1/3 of the tongue. The last visit in our clinic patient was given the adult referral to evaluate intraoral lesion but she never went to see the doctor for evaluation. A light coating of the dorsum of the tongue. Moderate crowding of both dental arches. Bilateral class I of occlusion, overjet 5mm, overbite 80%. Generalized supra and sub calculus on the mandible and generalized supra and localized sub calculus in mandible- posterior region.
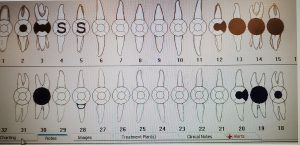
DENTAL CHARTING
Missing teeth: # 16,17 and 32. Amalgam restoration: teeth #2-O, #3-DOM, #12- DO, #18-O,#20- DO. Resin-based composite: tooth # 28 class – V. Sealants – teeth # 4 and 5. Crown – teeth #13,14,15,19 and 30. No clinical or radiographic evidence of caries present.
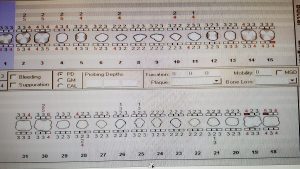
Gingival description and periodontal status
Gingiva is slightly inflamed, generalized pink but localized reddish-blue around the margin in the areas with crowns. Pocket depth generalized 2-3mm and localized 4-5mm. Moderate bleeding on probing.Recessions: teeth #2-5, 7,10,11 and #21,25,26,28,30. Periodontal type I, localized II.
DENTAL HYGIENE DIAGNOSIS
The patient is a periodontal type I- due to generalized 2-3mm pocket depth, gingiva slightly inflamed, and moderate bleeding while probing. Localized type II-due to bone loss and connective tissue attachment, subgingival calculus, measurable pocket depth (4-5mm)with moderate bleeding on probing. Generalized recessions. No mobility.
DENTAL HYGIENE CARE PLAN
The patient will come in 2 visits. First, visit educated patients on tooth brushing and demonstrated the Bass method. Expose 4HBWs and evaluate the x-ray. Scale quadrants I and IV, use anesthetics if needed. For the next visit: reviewed brushing technic with the patient. Introduced the second aid of flossing. Continue scaling quadrants II and III, use anesthetics if needed. Engine polish and 5% fluoride varnish.
IMPLEMENTATION- TREATMENT –INCLUDE ALL VISITS
First visit: EO/IO examination, dental and periodontal chart, calculus detection. Exposed 4HBWs and discussed it with the patient. PI score – 1.0 fair. The introduced correct method of modified bass toothbrush technique. Started scaling quadrants I. Used ultrasonic powerline FSI-1000, to reach better subgingival areas I used slimline FSI- 1000, and in anterior teeth, crowding, interproximal areas I used thinsert. I managed to remove the calculus, but anyway there was some residual calculus in interproximal areas and I used 13/14 and 11/12 Gracey curettes. Second visit: Reviewed medical history, and OHI. The patient told me that she tried to use the toothbrush technique I taught. Based on the findings from PI score(0.9) patient was not able to remove plaque from interproximal areas, so I introduced the patient how to use floss correctly ( C shape and slightly go under the gum)and also talk about mouth rinses and recommended her to use an antibacterial mouth rinse. Next scaled quadrants II, III, and IV used the same instruments as the first time. Engine polish and applied 5% NaF varnish and gave the patient instructions. (do not brush or floss for 6 hours, don not use hot or crunchy food). Recall after 4 months. No referral was given to the patient.
REFLECTION
I believe I accomplished everything I planned and the patient left our clinic satisfied. Introducing the Bass toothbrush technique and flossing method ( C shape) were important in the patient’s education. By doing this case study I got additional information on medications and their side effects and how a condition such as high blood pressure and cholesterol affects a patient. I better understand the questions to ask the patient and implications I may see based on their medical history.