Case #1
A 50-year-old female patient presented for a re-care appointment in December 2021 and March 2022. She did not see any dental professional since 2019.
The patient presented with Type II diabetes (HbA1C 6.4), high cholesterol, frequent urination, and symptoms of G.E. Reflux. She is currently taking Metformin, Simvastatin, OTC Vitamin D, and Multivitamin complex. She took Aspirin in December 2021, but it was discontinued in March 2022 due to her physician’s recommendation.
The patient mentioned she required local anesthesia for all previous cleanings.
The home care routine included brushing with a powered toothbrush once a day, flossing occasionally, and rinsing with Antiseptic Listerine, 2-3 times a day.
The IO/EO revealed a slightly coated tongue, bilateral scalloped tongue, maxillary torus, and bilateral linea alba.
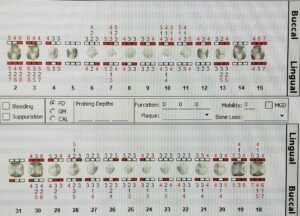
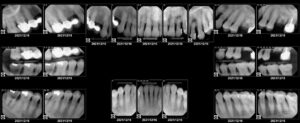
Upon assessment completion, an FMS was recommended. The patient presented with generalized suspicious decay, fractured teeth, generalized PD of 3-6mm, generalized subgingival, and localized supragingival calculus.
The FMS corroborated the clinical presentation. In addition, multiple areas of PAP, and dental decay under permanent restorations were found. The patient presented generalized bone loss of 15-33% and localized areas of >33%.
The patient presented twice for recare visits. The case value was heavy for both appointments with high caries risk and Stage III, Grade B periodontal classification.
A referral to the general dentist was provided to address the issues the patient has experienced. The treatment plan was developed based on the patient’s assessment and needs. It was recommended for the patient to continue using her powered toothbrush, and to change the brush head every three months. Additionally, a tongue cleaner and a regular proxy brush were added to the routine. Superfloss was recommended, and Listerine Total Care or ACT was advised due to its higher concentration of fluoride.
Nutritional counseling was performed, and it was determined that the patient consumes a high quantity of lemon juice daily. Thus, it was recommended to stop the habit or reduce the quantity and frequencies. The bi-directional relationship between diabetes and periodontal disease was explained to the patient and an additional pamphlet was provided to the patient with information.
Whole mouth scaling with local anesthesia was advised. Previous notes revealed the patient had a bad experience with Lidocaine. Thus, Carbocaine was used via ASA, MSA, PSA, and Buccal, Mental, and Papillary infiltrations. Selective scaling was performed and compromised teeth affected by severe decay or major fractures were not scaled. These teeth were not scaled to prevent further exacerbation of the damage and to keep the patient comfortable. Engine polishing was recommended, and 5% NaF varnish was advised due to multiple restorations and recessions. On every visit, the attention was brought to the immediate need for a general dentist intervention due to the excessive caries lesions. The next recare hygiene appointment was recommended in 3 months.
Case #2
A 78-year-old male patient presented for an initial visit in February 2022. A patient presented with high cholesterol, high blood pressure, and type II diabetes. Current medications included Metformin, Repaglinide, Hydralazine, and Amlodipine. The patient was classified as ASA 3.
The main chief complaint of the patient was a dental cleaning, where he didn’t have one since October 2010. He also presented with partial upper and lower dentures which he had for about 40 years and been not been taking them out at night. His home care regimen included soft bristle tooth brushing with Colgate toothpaste and rinsing twice a day with Crest oral rinse.
His IO examination findings were gingival stomatitis on upper and lower arches, fistulas on #2-B,#3-L, and #32-MB apical regions of the teeth.
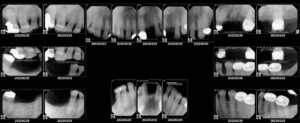
Dental and periodontal charting revealed ten clinically missing teeth, suspicious caries lesion, generalized PD of 1-3 mm and localized 4-5mm, and generalized subgingival calculus. The recommendations were to expose an FMS to obtain a more accurate diagnosis and to evaluate the three areas with fistulas as well as evaluate the bone loss.
FMS revealed PAP at root apex o f #2,3,32 and an additional site of a suspicious area of decay, Generalized vertical bone loss posteriorly, and horizontal bone loss anteriorly. The case value for the patient was heavy, with high caries risk, Stage III, Grade B.
Considering oral findings, at first, the patient was educated on the proper maintenance and use of his partial dentures. It was recommended to take the dentures out at night and soak them, as well as to clean them outside the mouth. The home care recommendations were the introduction to the modified bass method and superfloss due to teeth spacing and class 2 embrasure papillary spaces. During two visits of the whole mouth scaling the local anesthesia with ASA, PSA, buccal and mental infiltrations were administered, scaling one of the mouth per visit. Several teeth were not scaled due to them being compromised. Engine polishing was recommended to remove stains, as well as 5% NaF varnish due to high caries risk. A recare visit was recommended in 3 months’ time.
Arestin Case
The patient is a 20-year-old Asian male. Presented with no medical problems, medications, or allergies, as well as a non-drinker or a non-smoker. Classified as ASA 1.
His homecare routine only included powered toothbrushing twice a day with Sensodyne toothpaste. Also, he hasn’t been to the dentist for several years and never had radiographs done.
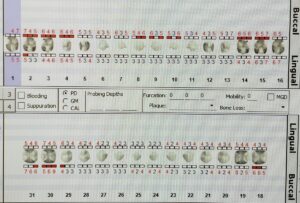
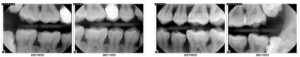
The patient presented with heavy subgingival and supragingival calculus buildup and generalized PD of 3-6mm and localized PD of 7-8mm. The 4BW was recommended for bone level evaluation to determine the extent of periodontal disease.
4BW were exposed and generalized 15% horizontal bone loss was recorded, as well as a localized area between #19-20 where it extended beyond 33%. Stage 3 Grade B was assigned to this patient.
Arestin Treatment was recommended to this patient considering his young age and the extent of periodontal disease at such young age.
With periodontal scaling some PD has reduced and sites of 29-DL (5mm), 18-MB(5mm), 9-MF(5mm), and 7-MF(5mm) were picked as sites for Arestin placement since they didn’t have major changes and still within range for Arestin placement. Additional PA of #7-9 was taken. Arestin was placed only after scaling was completed and tissues had 2 weeks to heal.
The patient has returned for evaluation in 5 weeks.
29 DL 5mm -> 4mm
18 MB 5mm ->3mm
9 MF 5mm -> 4mm
7 MF 5mm ->4mm
The following PD were recorded and changes were noted and the patient was informed of changes as well.