Case Study #1 –
Patient with Hyperthyroidism.
- Demographics:
-66 years old
-Caucasian
-Female
- Assessment:
– Patient had anxiety, hyperactive thyroid, arthritis, hypertension. The patient was taking medications: Methimazole – 20mg, Losartan – 100 mg, Metoprolol – 50mg, Escitalopram – 10mg. No known allergies. Vital signs: blood pressure 134/80 – hypertension stage I, pulse 76 beats per minute. Smoker for ten years, 3 cigarettes a day. ASA II.
– Last dental visit was performed on 11/2017, full mouse restoration was performed – multiple bridges and root canals, FMS was taken the same day.
– Extraoral findings: Multiple moles on the right check; Enlarges thyroid; TMJ small bilateral popping upon opening.
– Intraoral findings: Geographic fissured hairy tongue; Raised pink circular lesion 6mm diameter on the anterior of the tongue left to the midline, patient reports a history of trauma (biting on tongue) and without change 20+ years; On facial attached gingiva between #26 and #27 raised white sessile lesion 5mm wide and 4mm vertical, firm to palpation; Varicose veins on the ventral surface of the tongue; Dry mouth; Minor bilateral linea alba.
– Dental Assessment: Class of occlusion I; Anterior edge to edge bite.
– Moderate generalized gingival inflammation; Bulbous gingiva around #22. The patient had both maxillary and mandible round house PFM bridges. Porcelain fracture on the lingual side of #21 with exposed metal. #22 has a visible facial crack in the porcelain. Heavy subgingival calculus deposits detected on the mandible lingual side from #20 to #28. 4-6mm probing depth with moderate bleeding upon probing.
- Diagnosis of oral condition:
-Case value was determined to be heavy; Stage-III/ Grade-C periodontitis.
- Planning and Implementation:
-Exposed FMS radiographs.
Radiographic findings: Generalized moderate bone loss; Significant bone loss around #14 and #24-#25.
– Full mouth scaling and root planing performed using hand instruments with local anesthesia: two carpules of Carbocaine 3% used, delivered on the left and right mental infiltration, ASA, MSA and PSA with negative aspiration.
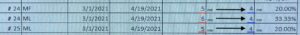
– Arestin placed on #24-MF, #24-ML, #25-ML; consent form signed and scanned, post-op instructions were given.
– Oral Hygiene Instructions:
The patient was advised to start using water floss with Crest Pro-Health anti-gingivitis oral rinse. Super Floss technique performed to keep areas under the bridges clean, patient understood and demonstrated the technique back. As an addition Genius Oral B proxy brush recommended especially for the mandible anterior area under the bridge.
– Referral given to Oral Surgent for evaluation of raised white sessile lesson on gingiva between #26 and #27; and raised pink lesson on the tongue.
- Evaluation:
– Treatment was performed within two visits. The patient presented for evaluation of Arestin in 6 weeks. Probing depths were improved by 1mm on #25 mesial side and 2mm on #24 mesial side. Gingival tissue on the previously treated areas had no more inflammation, not fluffy, looks pink, more stippled, very slight bleeding on gingival manipulation left. The patient was advised for a 3-month re-care visit.
- My reflection:
– As for a future hygienist, this case was a very valuable case to me. It was very important to think critically and make a fair decision about the treatment. The patient had many medical conditions and taking multiple medications which impact the oral cavity appearance and oral health. It was very important to find the right way of treatment to get the best possible outcome. The patient had severe periodontal disease and my goal was to stop the deterioration of the condition and to improve the state of the severely inflamed gingiva. Arestin was an auxiliary medicine to improve the most damaged areas. The treated areas on the evaluation appointment looked much better than before: no more fluffy-red inflamed gingiva, no more bleeding upon the gingival manifestation, the pink color of the gingiva, more stippled, and better snug the teeth. Arestin results were incredibly good – 1 to 2 mm improvement in the treated areas. It showed the best outcome can be. The patient responded to the treatment very well and very happy with the results.
Case Study #2 –
Patient with Seasonal Allergy.
- Demographics:
-34 years old
-Caucasian
-Male
- Assessment:
– The patient had seasonal pollen allergy; triggers are dust, fur; the patient gets sneezing effect. When needed, the patient uses Albuterol Sulfate inhaler – 2 inhalations. Vital signs: blood pressure 138/79 – hypertension stage I, pulse – 77 beats per minute. ASA II.
– Last dental visit 02/2015, dental cleaning and 4 bitewing x-rays were performed.
– Extraoral findings: TMJ – left side clicking during opening and closing.
– Intraoral findings: fissured tongue.
-Dental assessment: Class I of occlusion; Overjet 3mm; Overbite 50%.
-Above #14 in the area of the apex on gingiva from the facial side was detected hard, raised, round lesion 6 x 6 mm in diameter, painful when pressed; referral given for evaluation.
-Moderate generalized gingival inflammation; festooned gingival margin on the facial side of maxillary and mandible; generalized moderate BOP; inflamed and slight bulbous papilla on maxillary and mandible. Moderate/heavy calculus deposits detected interproximally on all mandible and posterior maxillary teeth, and on the lingual side of posterior teeth on maxillary and mandible. Moderate stains were presented on the gingival margin from the lingual aspect on the mandible and maxillary teeth. Generalized biofilm mostly located along the gingival margin. Plaque Index (PI) score: 1 – Fair.
- Diagnosis of oral condition:
Case value was determined to be heavy; stage II – Grade A periodontitis. Mild attrition on maxillary and mandible anterior teeth. Low caries risk – the patient has not had any caries in the past 36 months.
- Planning and Implementation:
– Exposed FMS radiographs.
Radiographic findings: #14 – Mesial root periapical pathology detected; generalized mild horizontal/vertical bone loss; calculus detected on #2-D, #4-M, #5-MD, #7-D, #8-M, #9-M, #12-M, #15-D, #18-MD, #20-M, #21-MD, #22-D, #23-M, #24-MD, #25-MD, #26-M, #29-M, #30-D, #31-M.
– Full mouth scaling and root planing performed using hand instruments with local anesthesia: two carpules of Lidocaine 2% epinephrine 1:100k delivered in areas: left and right PSA, MSA, mental and buccal infiltration with negative aspiration. Stains polished with pumice.
-Oral Hygiene Instructions:
Oral B E-toothbrush technique discussed. Flossing technique demonstrated, patient understood, agreed and performed back by the patient. Stim-U Dent recommended for some open interproximal areas.
– Referral given to evaluate wisdom teeth #1, #16, #17, #32; periapical pathology on the mesial root of #14.
- Evaluation:
– Treatment was performed in two visits. On the second visit on the previously treated areas, slight gingival inflammation was still present, but improvements can be seen: instead of moderate bleeding on gingival manipulation, only very slight bleeding left. The patient responded well to treatment. The patient was motivated and purchased the timer to keep the brushing process for the whole two minutes.
- My reflection:
– A patient with a seasonal allergy or asthma condition is one of the possible emergencies in the dental office. It was important to me as a future hygienist to treat this patient. One of the problem I’ve met is the use of epinephrine in the local anesthesia on this patient, as we don’t know what triggers asthma. Due to the mild seasonal allergy the patient had, the decision was to use the epinephrine for local anesthetics with precaution. During the whole appointment, the patient had an Albuterol inhaler on the counter. The whole procedure went very well without any incidents and with controlled bleeding. On the second appointment, the gingiva appeared pinker with less bleeding. The patient was very impressed to see the results and motivated to follow all the oral hygiene instructions and advices to keep oral health.
- PA x-ray of #14
- Pictures before:
-

-

-

- Pictures after:
-

-

-

Other Cases:
Colgate Home Whitening – Before & After