Case Study #1 / Patient with Hypothyroidism and Peri-implantitis
Demographics: The patient is 57 years old, Asian female.
Assessment: Patient has a seasonal allergy (red eyes and sneezing), takes Allegra. Patient had thyroid cancer, thyroid gland was removed in 2017. Patient takes Levothyroxine 88mg once a day before breakfast to prevent hypothyroidism. Last dental cleaning and x-rays were in summer 2021, last dental exam was in spring 2020.
Patient was concerned with exposed implant #30. Patient stated that she went to her DDS and DDS does not want to treat it right now.
Patient’s oral homecare consisted of toothbrushing 2x/day with an electric Oral-B and Sensodyne toothpaste. For interdental cleaning, patient used Water-pick 1x/week. Patient rinsed 1x/day with the prescription oral rinse for periodontitis.
Vital signs: BP-99/69 mm Hg, P 73. ASA 2.
Social Hx: non-drinker, non-smoker
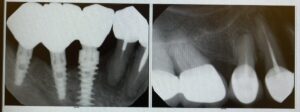
Dental assessment: #1, 4, 8, 10, 14, 16, 19, 29, 30, 31, 32 are missing. Bridges: #7-12 ( # 7, 9, 11, 12 are abutments), #13-15 ( #13, 15 are abutments), #18-20 (#18, 20 are abutments). #2, 3, 5, 6, 17, 27, 28 are crowns. #29, 30, 31 are implants
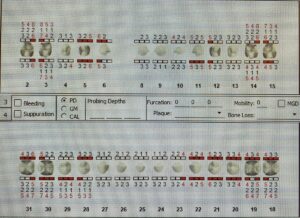
Gingival tissue was generalized red, enlarged, receded, soft, and shiny. Generalized moderate BOP. Generalized moderate recession. Mobility class I on #21, 22, 23, 24, 25. Periodontal classification was Stage II Grade B (based on x-rays).
Evaluation:
Treatment was performed in 2 visits. 4 PA x-rays were taken for evaluation of PAP and failing implant # 30. X-rays revealed PAP on # 5, 20, 27, 28; peri-implantitis on # 29-31. Patient was informed of the findings. Patient was concerned with the progression of the periodontal disease and feared losing more teeth and implants. Continuation of the prescribed oral rinse, as well as Chlorhexidine rinse, was recommended. Referral for evaluation of PAP and peri-implantitis was given to patient. After the removal of heavy calculus deposits from the lower anterior teeth, embrasure class III was noted. Patient was introduced to flossing with tufted floss in the embrasure space and under the bridges. Patient experienced dentinal sensitivity to the exposed root surfaces during scaling with Cavitron. Reviewed and explained the importance of using Sensodyne or other desensitizing toothpaste and the proper technique of brushing with an electric toothbrush. As per DDS, did not probe or scale the failing implants. Recommended recare was 3 months. A possible side effect of Levothyroxine is dry mouth. Patient had a history of decay and losing teeth due to decay. Currently, patient had a high risk for decay also due to exposed roots. Patient education was an important step during the treatment.
Case Study #2 / Patient with stent and GERD
Demographics: Patient is 63 years old, an African-American female.
Assessment: Patient did not have any allergies. Patient had stent placement in 2009. Since then, patient had been on the following medications for stent management: Aspirin 81 1x/day, Metoprolol 25mg 1x/day, Crestor 10mg 1x/day. Patient also had GERD and was taking on and off Prilosec 40mg. Patient had knee replacement surgery in 2009. The most recent hospitalization was on 8/22/2019 due to a knee replacement revision. No need for premed over 2years. Patient has not been to her MD in a year. Last dental cleaning and x-rays were in March 2020, last dental exam was in November 2019.
Patient’s oral homecare consisted of toothbrushing 2x/day alternating a medium manual toothbrush and electric Oral-B with Crest Gum Detox toothpaste. For interdental cleaning patient used tufted floss 2x/day. Patient rinsed 3x/week with Listerine and Periodex.
Vital signs: BP-135/83 mm Hg, P 78. ASA 2.
Social Hx: she drinks a drink/week, non-smokerOE: Linea alba bilaterally, fissured tongue, short lingual frenum, dry mouth due to meds, enlarged tonsils ( patient states it is always enlarged).
IE: Linea alba bilaterally, fissured tongue, short lingual frenum, dry mouth due to meds, enlarged tonsils ( patient states it is always enlarged).
Gingival tissue was generalized pink, receded, multiple missing papilla, non-stippled. Generalized light BOP. Periodontal classification was Stage II Grade B.

Evaluation:
Treatment was performed in 2 visits. Patient has not been to her MD in a year. Patient was told that it is important to go for annual physical examination due to multiple systemic conditions. Referral was given for annual physical examination. Patient had knee replacement revision surgery in 2019. MD did not recommended to take antibiotic premedication before dental treatment. Patient complained about experiencing dry mouth. Patient was educated that a possible side effect of taking multiple medications can be dry mouth. Recommended to drink a lot of water throughout the day. For pain management used Oraquix. Patient was also educated on flossing with string floss and toothbrushing with manual TB. She was using a medium bristle toothbrush and was concerned with the gum recession. The importance of using soft bristle TB was discussed. Recommended recare was 3 months.
Arestin
Demographics: Patient is 33 years old, an African-American female.
Assessment: Patient had no allergies. No meds. Patient was concerned with gums inflammation. Last dental exam and x-rays were in April 2021, last dental cleaning was in 2019.
Patient’s oral homecare consisted of toothbrushing 2x/day with an electric Burst toothbrush and Crest toothpaste. For interdental cleaning patient used toothpicks every time after food consumption. Patient rinsed 1x/day with TheraBreath.
Vital signs: BP-121/88 mm Hg, P 60. ASA 1.
Social Hx: non-drinker, non-smoker
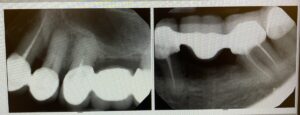
Radiographic statement: radiographic bone loss >15%, generalized calculus, incipient lesion on #3M, 4MD, 12D, 13MD, 14D. No PAP.
Gingival tissue was pigmented, papillary enlarged, bulbous, soft, smooth. Generalized heavy BOP. Periodontal classification was Stage II Grade B.
Evaluation:
Treatment was completed in 3 visits. During the second visit, Arestin was placed in previously scaled Q1. Placed Arestin at 4 sites: #2MB, #2ML, #3DB, #3DL. The probing depth before scaling was #2MB-6, #2ML-6, #3DB-7, #3DL-6. After scaling the probing depth decreased by 1-2mm already, so the measurement before the placement of Arestin was 5mm on all four sites. Patient returned for reevaluation after 3 weeks. After the reevaluation of the sites, the probing depth was 4mm on one site and still 5mm on three sites, which means Arestin did not decrease the probing depth.