The patient under examination was a 66-year-old Caucasian male who presented to our facility seeking a dental cleaning because his front teeth are sensitive. The patient had a medical examination in August of 2023. During the initial appointment, the patient’s blood pressure was recorded at 140/80; P:75 bpm, indicating Stage II hypertension. ASA III. The patient reported a family history of high blood pressure but is not currently taking any medication for it. The patient is allergic to penicillin. The patient has type II Diabetes and takes Metformin 1000mg twice a day, Glipizide 5mg/twice a day, Farxiga 10mg/once a day, and Rybelsus 14mg once a day. The last HbA1c was 7.5. The patient was diagnosed with Myositis on 8/17/2023. Myositis is a condition that can cause muscles to become weak, tired, and painful. The word myositis means inflammation in muscles. The patient is taking Methotrexate once a week, 6 (tabs), and folic acid daily to treat the condition.
Additionally, the patient reported does not drink, smoke, or use any recreational drug. The patient’s last dental visit was two and a half years ago for periodontal maintenance. The patient’s oral home care routine includes using a medium-bristled toothbrush with fluoride toothpaste. Flosses something; no mouth rinse or tongue cleaner use.
A comprehensive examination of the external and internal oral cavity was conducted during the patient’s initial visit. Multiple macules around the forehead, scalp, and face were observed. The patient reported that it was due to sunspots. Multiple red patches 2×2 inches are also present in the occipital area, right on the hairline and around the scalp. The patient has no uvula (scar tissue remains). The uvula was removed 15 years ago due to sleep apnea. The patient presents a fissured tongue and bilateral mandibular tori, and light tetracycline staining is present. The patient stated he was on tetracycline medication as a child.
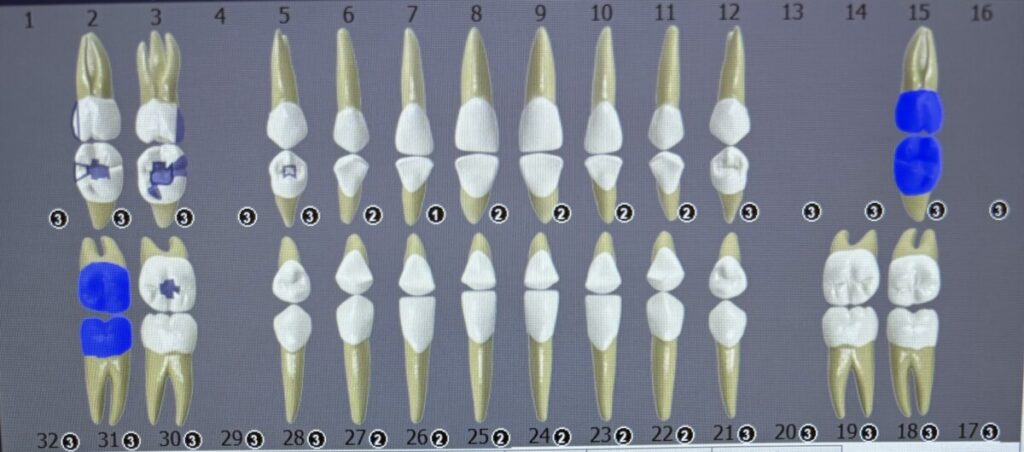
Dental charting was performed. The patient has a bilateral class I occlusion, 2mm Overjet, and 10% Overbite. Mobility is not present. The gingival margin is generalized pink with a slightly bulbous papilla, soft consistency, and shiny appearance. There is localized inflammation on the posterior teeth. The gingiva margin is rolled on the lingual anterior teeth, and there is generalized bleeding on probing.
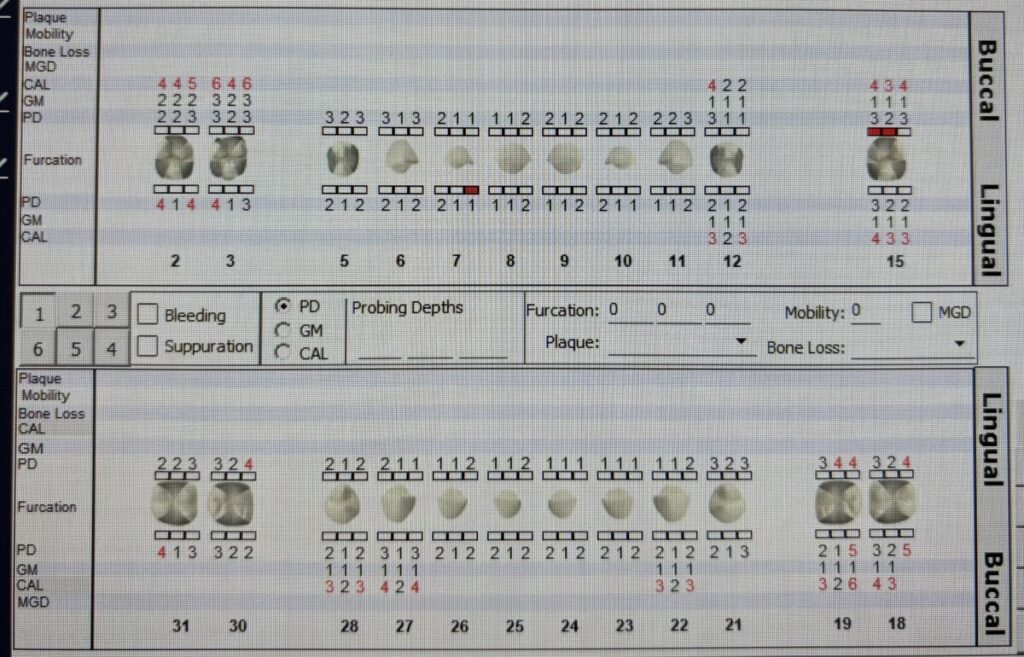
Periodontal charting was conducted. There is a generalized gingival recession of 1-2mm, generalized probing depths of 2-3mm, and localized 4-5mm on posterior teeth. The gingival margin is apical to CEJ. Heavy calculus and biofilm are present on anterior teeth. Plaque Score: 1.7 (fair) Case Value: Heavy Stain: Heavy due to tetracycline medication. Caries Risk: High based on CAMBRA and due to multiple restoration and medication intake with the side effect of xerostomia.
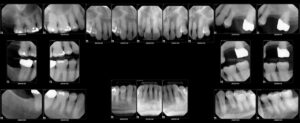
A Full Mouth Series of x-rays was also performed, which revealed radiographic evidence of calculus on tooth #19M, generalized less than 33% of horizontal bone loss, and a suspicious carious lesion on #2 and #12D. No Periapical pathology or jaw bone abnormalities were noted. Based on the radiographic evidence and periodontal charting, I classified the patient’s periodontal status as a periodontitis Stage II Grade C. The findings were shared and discussed with the patient. These findings indicated a significant level of periodontal disease and oral pathology that must be addressed to ensure the patient’s oral and systemic health. I needed to implement a comprehensive treatment plan that addressed these issues and prevented further deterioration of the patient’s oral health.
By closely monitoring the patient’s progress, I was able to provide exceptional care and ensure the patient’s continued oral health. For oral hygiene instructions, I advised my patient on the importance of brushing twice a day with Prevident 5000 toothpaste before bed and Biotene as a mouth rinse to prevent cavities and severe dry mouth by using the Modified Bass brushing technique taught during the visit and flossing twice a day. Also, I explained how crucial it is to maintain a healthy diet, avoid sugary food and beverages, and drink water frequently to prevent dry mouth and cavities.
Implementation
-
I completed exposure to FMS digital radiographs. The professor and I both demonstrated the radiographs to Miss M and explained to him the bone loss and the amount of subgingival calculus observed interproximal. He understood better how the calculus contributed to her bleeding and periodontal disease.
- I recomment to use a sensodyne toothpaste and Listerine Sensitivity Mouthwash daily.
-
The C- shape flossing method was introduced, and the importance of flossing least once daily was reiterated. Upon demonstration. The patient performed well.
-
Debridement of the Q4 quadrant with ultrasonic and hand instruments. Oraqix(2.5% lidocaine and 2.5% prilocaine ) was used for pain management.
-
An adult referral was given to a physician for hypertension stage II.
Evaluation of Care
In summary, evaluating care for a patient with heavy calculus, bleeding gums, diabetes, xerostomia, and sensitive front teeth involves addressing oral hygiene, managing sensitivity, and providing a prognosis based on their overall health and adherence to recommended care.