Patient Profile
- 53 year-old black male
- Last dental visit – June, 2018
- Last dental radiographs – June, 2018, 4 BWs
- Patient reports to brush with manual brush twice a day with Colgate toothpaste, uses Listerine oral rinse once a day, flosses rarely (once a week)
Chief Complaint
Patient states that “I’m here for a dental cleaning. I have residual gums and sensitivity, but overall I feel good about my teeth.”
Health History Overview
- Patient said that he has high blood pressure and he is under the care of doctor
- First reading: 163/117, Pulse 89
- Second reading 5 minutes later: 178/115, Pulse 87 – Stage 2 Hypertension
- Patient was present with medical clearance from his doctor. Doctor stated that the patient has no contraindications to perform the dental hygiene service and does not require antibiotic pre-medication
- Patient takes prescribed Amlodipine 5 mg once a day
- Non drinker, non social smoker
- ASA II
High Blood Pressure
Blood pressure (BP) describe as a force of your blood against your artery walls and consists of two numbers: systolic and diastolic. Systolic number is higher and corresponds with pumping the blood, where diastolic is your blood pressure at rest, between beats
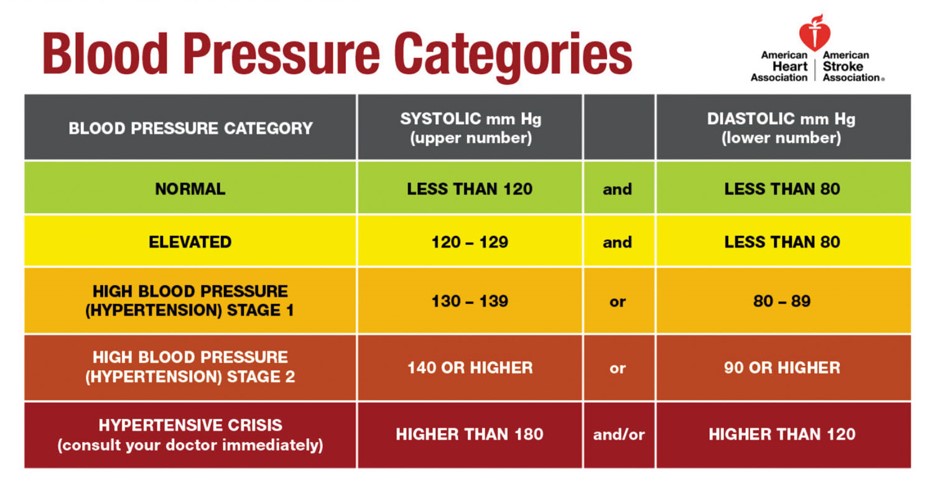

- Even if BP readings are dangerously high, there could be no symptoms or signs
- Primary high BP is the most common and develops over time as you age
- Secondary high BP could be caused by many conditions, including kidney problems, thyroid problems, obstructive sleep apnea, adrenal gland tumors, and others
- High BP could lead to heart attack, stroke, heart failure, kidney failure, vision loss
Risk factors
- Age (until age 64 more common in men, after age 65 in women)
- Race (common among African heritage)
- Family history
- Being overweight or obese
- Low physical activity
- Tobacco, alcohol
- Too much salt, too little potassium in diet
- Stress
Management of high BP
Lifestyle and diet changes are recommended, as well as physical activity. In addition to above doctor may prescribe following medications:
- Thiazide diuretics
- Angiotensin-converting enzyme (ACE)
- Calcium channel blockers
- Alpha blockers
- Alpha-beta blockers
- Beta Blockers
- Aldosterone antagonists
- Renin inhibitors
- Vasodilators
- Central-acting agents
Patient is taking Amlodipine (Norvasc). It’s a calcium channel blocker – this helps to relax the muscles of blood vessels. Calcium channel blockers are recommended as a first treatment for older people, people with diabetes, kidney disease, and people of African heritage.
Dental Hygiene Management
Many patients with HBP medications (including amlodipine) may experience orthostatic hypotension, altered taste, and xerostomia. Calcium channel blockers are reported to cause gingival hyperplasia and erythema multiforme. Common drug interactions: Aspirin, NSAIDs, erythromycin, clarithromycin. To manage the orthostatic hypotension patient should be seating in upright position, also patient should take his time to stand up, no fast motions. For patients reporting xerostomia no alcohol mouth wash should be suggested. Multiple mouthwashes designed for dry mouth could be recommended (Biotene Dry Mouth Oral Rinse, Act Dry Mouth), as well as sugar-free gums (Xylitol). Dentist could prescribe medications such as Salagen, Evoxac to stimulate saliva flow.
Radiographs
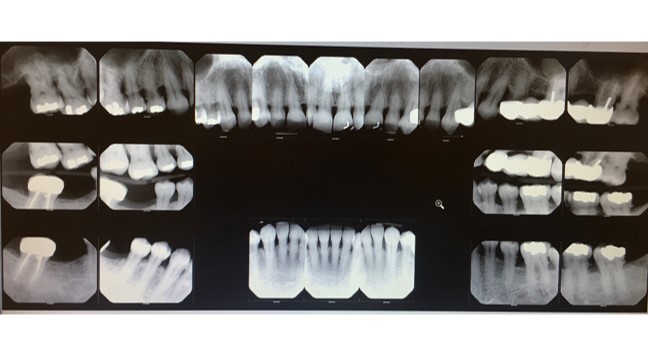
Generalized calculus; caries #2D, #4D, #15D, #19D; generalized slight horizontal bone loss, localized moderate to severe bone loss in sextants 1, 3 & 4.
Summary of Clinical Findings
EO: birth marks and small macules scattered around the face. Patient has a history of running nose. Patient has mobile enlarged submandibular lymph nodes – asymptomatic
IO: erythemic throat
Occlusion: class III on the right side, class II on the left side. Attrition #24, #25. Overjet 3mm, overbire 20%. No mobility
Generalized heavy subgingival deposits, generalized moderated supragingival deposits
Dental Charting
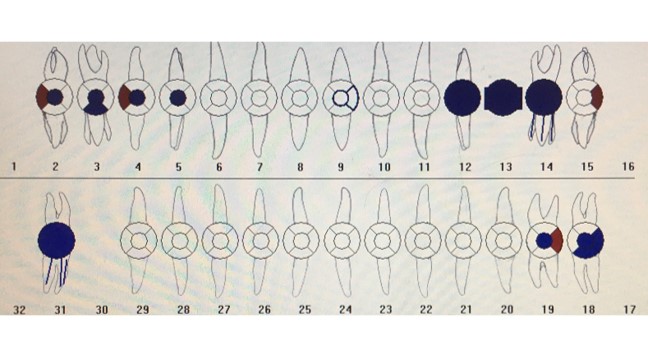
Missing teeth #1, #13, #16, #17, #30, #32
Amalgam restorations #2O, #3OL, #4O, #5O, #18DOB, #19O
Composite #9DO
PFM #12, #14, #31
Pontic #13
Caries Risk Assessment
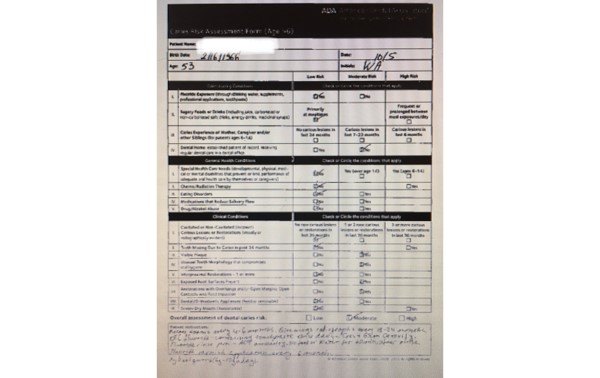
Decay noted clinically: #2D, #15D. Decay noted on radiographs: #4D, #19D
Gingival Description & Periodontal Status
Gingiva shows generalized pink color, soft, shiny, slight BOP, blunted papillae in the posterior region, few papillae are missing in the UR molar region
Periodontal Charting
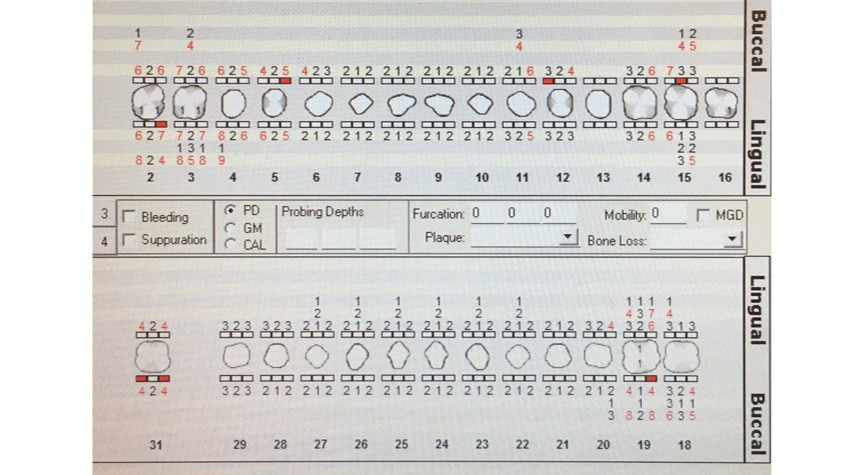
Multiple areas of gingival recession is noted. Low BOP. No mobility, Grade I furcation #2, #3, #19. Increased PD in sextants 1,3 &4
Dental Hygiene Diagnosis
Perio II stable periodontitis (localized III-IV) due to increased 4-7 mm PD (CAL up to 9mm), low BOP, Grade I furcation (#2, #3, #16, #19), and radiographic evidence of slight to severe bone loss.
Patient reported sensitivity, multiple areas of exposed cementum was noted and patient was expressing sensitivity upon exploring.
Caries were noted clinically and on radiographs. Due to exposed dentin and visible plaque patient is at moderated caries risk.
Dental Hygiene Care Plan
Visit one: complete assessment, obtained treatment plan consent, expose FMS, OHI Modified bass technique, scale UL and UR with ultrasonic and hand instruments.
Visit two: reevaluation of UR and UL, discuses possible Arestin treatment with patient and obtain consent, OHI on interdental aids (floss), scale LL with ultrasonic and hand instruments.
Visit three: reevaluation of LL, OHI on interdental aids (floss threader) and discussion on benefits of fluoride in toothpaste and mouthwash, scale LR with ultrasonic and hand instruments, engine polish with medium grit paste, apply 5% Fluoride Varnish.
Implementation
Visit one:
Completed assessment, obtained treatment plan consent. BP163/117, Pulse 89. Patient was present with medical clearance form due to HBP.
Patient was recommended: to use xylitol (6-8g/day) gum or candies. OTC with fluoride were recommended: Crest Gum Detoxify with Stannous fluoride 0.454%, ACT anticavity mouthwash with Sodium fluoride 0.05%. Application of fluoride varnish every 4-6 month.
Exposed FMS – findings were discussed with patient, referral form was given to the patient. PI fair. OHI Modified Bass technique – patient was able to demonstrate the technique and was corrected, asked if he has any questions. Scaled UR and UL quadrants with ultrasonic and hand instruments. No rescales.
Visit two:
No changes in medical history. BP 152/93, Pulse 88.
Evaluated of UR and UL quadrants, gingiva showed decrease papillae inflammation, less BOP. No residual deposits were found. PI fair with improvement due to corrected brushing technique. OHI floss – patient was able to demonstrate the technique and was corrected, asked if he has any questions. Scaled LL with ultrasonic and hand instruments. No rescales.
Arestin
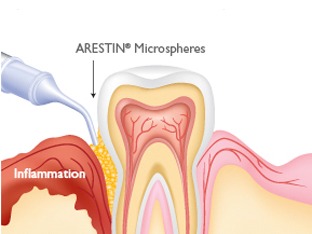
Arestin placement was recommended, discussed and accepted by patient. Patient had Arestin placed on 13 sites ranging from 5-7mm pocket depths on UL and UR quadrants 1 week after first debridement visit. Patient reported the placement was completely painless. Post instructions were given to the patient. Reevaluation was done in one month after placement. Generalized 1-2mm reduction in pockets depth was noted, patient was informed about successful treatment.
Visit three:
No changes in medical history. BP 143/102, Pulse 82.
Evaluated of LL quadrant, gingiva showed decrease papillae inflammation, less BOP. No residual deposits were found. PI good with improvement due to corrected brushing and flossing technique. OHI on floss threader for pontic #13 – patient was able to demonstrate the technique and was corrected, asked if he has any questions. Scaled LR with ultrasonic and hand instruments. Polished with medium grit paste. Applied fluoride varnish 5%. Recare 3 month.
Evaluation of Care
With each visit I noticed improvement on plaque index, I think patient significantly improved his brushing technique and now considers using floss and floss threader daily. My prognosis is that patient will be able to maintain daily oral hygiene and will stabilize his inflammation.
I also think with constant use of fluoride products patient will stabilize his sensitivity and significantly reduce the risk of caries.
Referrals
Referral was given on decay due to clinical and radiographic evidence. Chipped amalgam was noted on #18 and patient was referred to general dentist (restorative care). Also due to high PD, generalized horizontal bone loss, recession, and furcation patient was referred for evaluation to periodontist.
Continued Care Recommendations
Patient needs 3 month recare schedule. This patient was present with deep periodontal pockets and even with good oral hygiene he still would need 3 month reevaluation of his condition so it can get stable.
Final Reflection
This patient seemed to be open to learning everything about home oral hygiene. I was able to demonstrate every aspect of it and he always was engaged in re-demonstrating techniques.



