Case Study 1:
32 year old, African American male. Considered ASA I, non-smoker and social drinker. Presented with a chief complaint of wanting a “regular cleaning” but stated that he had a “horrible” past dental experience. Patient’s dental charting included several restorations of both amalgam and resin-based composite material. Periodontal probing classified patient as a generalized type II: slight periodontitis with localized type III: moderate periodontitis. There was moderate inflammation and bleeding upon probing. Patient presented with 2-3mm recession on both tooth #9 and 24. Generalized heavy subgingival calculus was present throughout the mouth. I exposed a full mouth series on this patient and it confirmed generalized horizontal bone loss of about 2mm in the posterior with localized 3-4mm vertical bone loss in the anterior aspect as well as the first mandibular molars. Therefore, my instructor and I, established a differential diagnosis of NUP: necrotizing ulcerative periodontitis. The patient disclosed that a couple of years ago he had a “surgery” performed by his dentist. The patient recalled having parts of his gums removed. When I asked for the dentist’s name to call for further information, the patient informed me that the dentist is in prison for insurance fraud. Therefore, I was not able to get more information about this patient’s past dental history. This patient was selected for Arestin placement due to pocket depths.
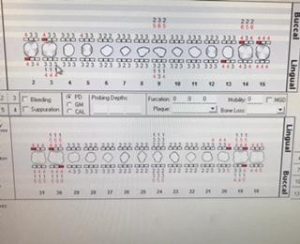
Image shows clinical attachment loss due to differential diagnosis of NUP periodontal disease.
I placed Arestin in 8 sites and was more than thrilled with the results when the patient came back for evaluation.
| Tooth site | Pre-Arestin | Post-Arestin |
| #14D | 5 | 3 |
| #15M | 5 | 3 |
| #19D | 6 | 5 |
| #19M | 7 | 4 |
| #20D | 5 | 4 |
| #20M | 5 | 4 |
| #21D | 5 | 3 |
With the patient’s permission, Arestin was placed by another student in other sites with deep probing depths. Those sites had similar results. I believe the patient got over his dental fear and began to focus on maintaining his teeth. Patient did not previously floss. For home care I taught flossing as well as introduced an electric toothbrush. I scaled with hand instruments and the ultrasonic. I also placed two sealants on this patient where he did not have restorations. I also engine polished with fine paste and applied 5% sodium fluoride varnish.
This patient was originally seen October 20th, 2017. He returned to our dental hygiene clinic in February 2018 where I treated him once more. This time, the patient had minimal calculus deposits and overall less bleeding. The patient’s probing depths were as follows…
Overall, I was very happy with this patient’s progress and I will continue to treat him if possible. I am still in contact with this patient and have established a dental relationship with him.
Case Study 2:
24 year old, Asian male. Considered ASA I, non-smoker and social drinker. Presented with a chief complaint was of wanting to “get rid of the yellow stains on front teeth”. Patient’s dental charting included one resin-based composite material, two amalgam fillings and partially erupted #17 and 32. Periodontal probing classified patient as a generalized type I: gingivitis with localized type II: slight periodontitis. There was moderate inflammation and bleeding upon probing. Patient had bright yellow supra calculus deposits on mandibular anterior teeth, almost neon yellow. Generalized heavy subgingival calculus was present throughout the mouth. I exposed 4 horizontal bitewings on this patient as well as a PAN x-ray. Bitewings and PAN both showed partially erupted 3rd molars. As a result of the positioning of #32, a carious lesion was forming on the distal of tooth #31. Therefore, I referred this patient to an oral surgeon for evaluation of wisdom teeth as well as possible caries.
Here is a photo of his calculus before scaling…
and after scaling…
For home care, I went over flossing with this patient, especially because of his crowded anterior teeth. I scaled the patient’s teeth with hand instruments and the ultrasonic. At the patient’s second appointment his plaque score decreased .50 from 2.60 to a 2.10. Patient tried to incorporate flossing and use Listerine Antiseptic Mouthwash. After scaling, I engine polished with fine paste and applied 5% sodium fluoride varnish.