Case Study #1 – GERD and Arestin
The patient under examination was a 38-year-old Asian male who presented to our facility seeking a dental cleaning. The patient has not had a dental visit in over five years, but had a medical examination in August of 2022. During the initial appointment, the patient’s blood pressure was recorded at 141/51 with a heart rate of 69 bpm, indicating Stage II hypertension. The patient reported a family history of high blood pressure, but is not currently taking any medication for it. Additionally, the patient reported a regular consumption of at least six servings of beer per week, daily use of e-cigarettes and cigarettes, and exhibited bleeding gums during toothbrushing. The patient’s oral home care routine includes using a soft-bristled manual toothbrush with Colgate Triple Action and Sensodyne twice daily, as well as flossing as needed. The patient also mentioned experiencing teeth grinding during the night and sometimes in the morning. Given this information, it was imperative that I thoroughly evaluated and addressed the patient’s oral health needs, while also considering the potential effects of his lifestyle habits and medical history.
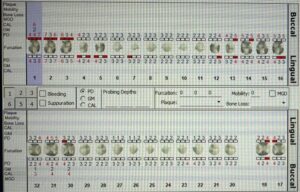
During the patient’s initial visit, a comprehensive examination of the oral cavity was conducted, revealing generalized attrition and exposed dentin on both maxillary and mandibular anterior teeth. Additionally, the patient presented with generalized reddish pink soft spongy tissue, slightly bulbous pyramidal interdental papillae, and generalized bleeding upon probing of the posterior teeth. A Full Mouth Series was also performed, which revealed a Heavy Stage III Grade C case value due to the presence of generalized radiographic evidence of calculus, furcation involvement (Class I and II), generalized 15% RBL, localized 30-50% RBL on the first molars, and a suspicious occlusal carious lesion on #14. These findings were indicative of a significant level of periodontal disease and oral pathology that was addressed in order to ensure the patient’s oral and systemic health. It was essential that I implemented a comprehensive treatment plan that addressed these issues, and prevent further deterioration of the patient’s oral health.
The patient returned for an additional three visits to complete his treatment plan, during which he reported “mostly” adhering to the C-Floss Method. However, it was emphasized to the patient that flossing at least once daily was crucial to achieving optimal treatment outcomes. During the second revisit, the patient’s probing depths indicated that he was a suitable candidate for Arestin Placement. After providing detailed information about the benefits of Arestin in reducing periodontal pocketing, the patient provided consent for placement on tooth #3, specifically on the DB (7 mm), MB (6 mm), DL (6 mm), and ML (6 mm) surfaces. The patient received post-operative instructions, which included avoiding brushing, flossing, and mouthwash use for 12 hours and waiting at least 10 days before using interproximal aids. By following these recommendations, the patient can maximize the results of the treatment and achieve a healthier oral environment.

During the patient’s first two revisits, no notable changes in their medical history were reported. However, during the third visit, the patient reported developing Gastroesophageal reflux disease (GERD) and subsequently started taking Pantoprazole (Protonix). It is important to note that Pantoprazole can have oral side effects, such as fruit-like breath odor, sore throat, and the development of sores, ulcers, or white spots on the lips or in the mouth. As a result of the patient’s new condition, his intraoral examination included inflamed red tonsils. The patient’s treatment was successfully completed during the third visit, and they were advised to return for a limited focus visit after 4-6 weeks to re-evaluate the probing depths of tooth #3. By closely monitoring the patient’s oral and medical conditions, I was able to provide the best possible care and ensure their long-term oral and systemic health.
During the limited focus visit, the patient’s probing depths exhibited a significant improvement, as follows: the DB probing depth reduced from 7 mm to 4 mm, the MB from 6 mm to 4 mm, the DL from 6 mm to 4 mm, and the ML from 6 mm to 4 mm. The patient was pleased and impressed with the effectiveness of the noninvasive and quick procedure, which resulted in such remarkable improvements. By closely monitoring and following up on the patient’s progress, I was able to provide exceptional care and ensure the patient’s continued oral health.