Case #1: Arestin and medically compromised patient
E.B., 76 years old, Caucasian female, Heavy/Type II.
ASSESSMENT:
A. Patient health history and vital signs, ASA
The patient has a well-controlled high blood pressure. Her vital signs were normal for her: BP measured 140/73 and pulse measured 58. Patient is taking Benicar (Olmesartan – antihypertensive drug) 100mg/1x day for six years. This is sometimes create a dry mouth and/or fruit-like breath odor side effects, which may modify the oral cavity or patient treatment.
The patient’s ASA classification is 2. She is a nonsmoker. No premedication, except Benicar, are needed.
B. Oral Pathology
Clicking of the patient’s temporomandibular joint from the right side with no pain was identified upon extra-oral examination. In addition, the patient has bilateral linea alba, red macule on the hard palate and white-coated tongue. No changes were indicated upon revisit appointments.
C. Dentition
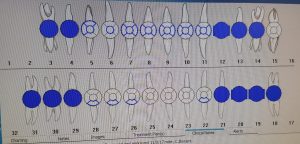
The patient has class I occlusion, overjet 3mm, overbite 30%. Generalized recession around 2mm. Localized prosthesis, bridges and crowns. Cantilever bridge on teeth #13, 14. Patient is missing teeth #1, 2, 16, 17, 32.
The above findings were identified without radiographs. However, FMS (20 films) was recommended.
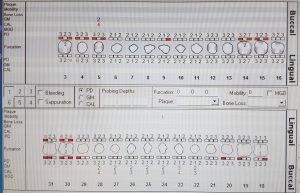
D. Periodontal
The patient is a periodontal case type II. The average probing depth was 4 mm with a few 10mm pockets on molar areas. Patient had severe bleeding upon probing, and severe inflammation. The patient’s generalized gingiva appears pale pink in color, pyramidal, firm, texture, bulbous (localized posterior). Generalized recession around 2mm.
Based upon the assessment, the patient is appropriate for Arestin. She has probing depths ≥ to 5 mm with BOP and presence of radiographic bone loss.
E. Oral Hygiene
The patient had an initial plaque score of 1.5 and a revisit plaque score of 1.2. The patient had generalized supragingival and subgingival calculus deposits, mostly interproximal. The patient has most of her plaque and calculus interproximal areas, so based on these findings, I demonstrated proper flossing technique in order to better access the interproximal areas. Because the patient has very tight contacts between her anterior teeth, I recommended wax-tape floss for her natural teeth and superfloss for her bridges and crowns. During our next visit, I demonstrated a Modified Bass tooth brushing method with a soft manual toothbrush (the patient was used to a medium-bristled toothbrush). Also, the patient had difficulty reaching posterior areas during brushing, and I accordingly introduced a single tufted toothbrush.
The supplemental aid demonstrated to the patient was a tongue scraper.
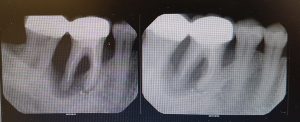
F. Radiographs
The patient had no history of dental x-ray. I performed FMS for the patient. Radiographs revealed impacted tooth #17, furcation #30, residual root tip #12. Patient presented with generalized moderate alveolar bone loss and supported placement for Arestin. Also, patient presented advanced bone loss between teeth #2 and #3.
G. Other findings
Patient is a nonsmoker and does not drink alcohol. One more factor that might affect the patient’s dental health that the patient is taking Benicar (antihypertensive drug) daily for six years – common dry mouth causes in adults.
TIME:
The patient stated that her last dental cleaning was approximately 2 years ago. This was not an appropriate amount of time for this patient. Because the patient is a heavy case value and type II periodontal classification, she requires more frequent visits to monitor and improve her oral health – three month recall interval is more beneficial for her.
TREATMENT MANAGEMENT:
During the patient’s initial visit, all assessments were completed. This was documented and was to be re-evaluated at the next visit. Patient was given a referral to a general dentist for restorations and caries-evaluation appointment. The patient was disclosed and received a plaque score of 1.5. OHI: taught the patient the correct flossing technique with wax-tape floss to access interproximal areas where plaque was most heavily accumulated. In addition, I showed the patient correct using of superfloss for her bridges and crowns. UR and LR quadrants were scaled using the ultrasonic and hand instruments.
VISIT 2
During the second visit, I re-evaluated the EO/IO findings and gingiva, patient’s right side of the mouth was less inflamed and bulbous. Also, I noticed bleeding reduction. Her plaque score showed an improvement – it was 1.2 (where on a previous visit the plaque score was 1.5). The patient responded very well to the wax-tape floss recommended in the prior visit. I also reviewed superfloss technique with the patient and introduced the Modified Bass tooth-brushing method. I then re-evaluated the previously scaled quadrants for residual calculus and scaled the UL and LL quadrants with ultrasonic and hand instruments. At the end of the visit, I applied polish and Varnish (5%) treatment.
In addition, three sites for Arestin treatment were choosing on previous scaled quadrants. Arestin was placed on the DB and DL of #4, and the DL #30. Post op instructions were given to the patient and she was to return in 6 weeks for re-evaluation.
VISIT 3
Limited focus visit – just re-evaluation of Arestin placement. #4DL 7 mm (no changes), #4DB 5mm (no changes), #30 DL 4mm (last time the probing depth was 5mm). I noticed less bleeding on probing. #30 DL – decrease pocket depth.
Patient on three-month recall.
EVALUATION:
The patient was very interested in the new flossing method I taught and the new type of floss (superfloss) I showed, and she was very excited to try it as part of her daily oral hygiene routine. She was especially interested when I showed her the calculus that presented in her mouth – interproximally, in the mandibular lingual anterior areas. The patient was further interested when I showed her plaque accumulation after disclosing. She became particularly attentive to her problem areas, which included interproximal. She was very motivated to learn flossing technique when she could see colorful plaque in her mouth. This is positive reinforcement because her technique needed to be modified, especially for posterior areas with her bridges and crowns. After completion, the patient noticed a difference – her teeth were smoother and felt cleaner.
At the initial visit, the patient had severe inflammation and severe bleeding upon probing with pale pink, firm, localized bulbous gingiva. After completion, the inflammation was minimized, as was the bleeding.
Besides, after Arestin placement I noticed decrease in pocket depth. There was a 1 mm decrease in the DL of #30. There has been some improvement, which made my patient happy.
Case #2: Periodontitis
V.T., 48 years old, Caucasian female, ASA I.
Patient came to appointment for routine dental cleaning. Patient’s main complaint was advance bleeding when she brushed her teeth. Patient was not taking any medications and did not have any medical conditions.
An intraoral examination revealed draining fistulas with abscess swelling around teeth #30, #19, #12. The gingiva was generally inflamed, bulbous, and bluish in color. Patient had advanced bone loss in her posterior areas. Patient was sent for exposed FMS, and the x-ray images showed generally present bone loss, and localized aggressive bone loss in the posterior areas. Patient needed immediate periodontal evaluation and treatment. Patient was given referral to periodontist.
Scaled anterior areas with ultrasonic and hand instruments. Patient was given letter stating that she needed periodontal treatment before resuming any other Dental Hygiene procedures.
Case #3: Tobacco-associated heavy deposits
J.A., 29 years old, Caucasian male, Heavy/Type II.
ASSESSMENT:
A. Patient health history and vital signs, ASA
The patient had no significant findings in his medical history. His vital signs were within normal limits: BP of 119/76 and pulse of 84. The patient is a heavy smoker. ASA classification is 2. No premedication are needed.
B. Oral Pathology
The patient has a solid raised papule on the left side of the mucobuccal folds. He also has three small petechiaes on the left side of the floor of his mouth, and bilateral linea alba. In addition, the patient has the scalloped green-coated tongue. No changes were indicated upon revisit appointments.
C. Dentition
The patient has class I occlusion, a 4 mm overjet, and a 50% overbite. He has composite restorations on occlusal surfaces of teeth #3 and #13, and an amalgam on occlusal surface of tooth #15.
The patient is missing teeth #1, #16, and #32. Tooth #4 has a fracture. Teeth #6, #11, #22 and #27 have attrition. Also, the patient has abrasion on teeth #5, #8, and #30.
The patient has a suspicious carious lesion on the buccal surface of teeth #17 and #4.
D. Periodontal
The patient is a periodontal case type II. The average probing depth is 3-4 mm with moderate bleeding upon probing and moderate marginal inflammation. A probing depth of 4 and 5 mm was recorded around most of the molars and anterior maxillary central incisors. The generalized gingiva was pink with red color on cervical third, inflamed, bulbous, firm, non-stippled, and with localized gingival recession on the buccal surfaces of teeth #3, #11, #15, #18, and #27.
Based upon the assessment, the patient is not appropriate for Arestin.
E. Oral Hygiene
The patient had an initial plaque score of 2 (poor) and, upon revisit, plaque scores of 1.8.
The patient had generalized supragingival and subgingival calculus deposits, mostly interproximal. Supragingival calculus was also present on the lingual surface of tooth #23 through tooth #26. The patient is a heavy case value, with medium extrinsic stains. Based on the findings, after discussing with the patient, I demonstrated how to properly floss. The patient had a high accumulation of interproximal plaque. The patient’s plaque score was 2 on this visit. Upon his next visit, the plaque score improved to 1.8. Due to the fact that the patient disliked brushing his teeth, I recommended using an electric toothbrush (trying to make things as easy as possible for the patient). We discussed the general toothbrushing technique for an electric toothbrush, including that it important for the patient not to scrub with electric toothbrush, or, otherwise, recession will occur even faster. I also introduced the tongue scraper, which I demonstrated as a supplemental aid.
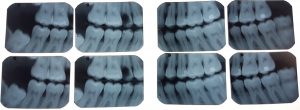
F. Radiographs
The patient stated that he had 4BW dental radiographs about 7 months ago and did not take any other x-ray films form many years.
Due to suspicious areas, I performed 4 horizontal bitewings for the patient and digital panoramic x-ray. Radiographs revealed that teeth #1, #16 and #32 are impacted. Tooth #4 had gross decay and also decay area was present on tooth #17.
G. Other findings
The patient is a heavy smoker. Also, one more factor that might affect the patient’s dental health that the patient does not like to brush his teeth on regular bases.
TIME:
The time interval between the last dental hygiene recall and today’s visit was 5 months. Due to periodontal type II and dislike of dental hygiene home care, the patient was on a 4-month recall schedule.
TREATMENT MANAGEMENT:
At the initial visit, I reviewed the patient’s medical history and vitals, and performed extraoral and intraoral exams. During the EO/IO exam, there was a finding of papule on the left side of his mucobuccal folds. The patient also had three small petechiae on the left side of the floor of the mouth, and bilateral linea alba. Additionally, the patient had a scalloped green-coated tongue. This was documented and was to be re-evaluated at subsequent visits. While completing the dental charting, I noticed a fractured crown on tooth #4 and a suspicious carious lesion on tooth #17. This prompted me to give the patient a referral to a general dentist in order to evaluate these teeth. Also, a copy of 4 horizontal bitewing radiographs panoramic x-ray were given to the patient. During the first visit a full mouth probing was completed. The patient had moderate bleeding and moderate inflammation upon probing with case type II. Calculus detection was completed, with classification established as a heavy case value; the extrinsic stain was medium. After discussing with the patient, it was evident that he had interproximal and anterior lingual plaque, especially on the mandibular arch. The overall plaque score was 2, which is poor. I discussed with the patient the results of his plaque score and what the visible red areas meant in relation to his oral hygiene. I explained to the patient that his flossing technique was not working well for him. I taught the patient the correct flossing technique to access the interproximal areas where the most plaque had accumulated. I demonstrated the “C” shape curved motion to access all areas of the tooth to make the floss disappear under the gums. Finally, on this visit I also scaled LR quadrant with ultrasonic and hand instruments.
VISIT 2
During the second visit, the extraoral and intraoral examinations were re-evaluated; no change was observed. His plaque score showed an improvement – it was now 1.8 (where on a previous visit the plaque score was 2). I reviewed flossing with the patient. Because the patient told me that he does not like brushing his teeth. I thought that an electric toothbrush would be a better choice for him. I introduced an electric toothbrush and went over proper brush placement. Also, we discussed toothbrushes from Oral-B and Sonic Care and their prices. I then re-evaluated the previously scaled teeth. Then I scaled the UR, UL, LL (I did not touch tooth #4, because of the fracture on that tooth). I used ultrasonic and handscaled instruments. At the end of the visit, I polished and applied 5% varnish fluoride treatment.
The patient is on a four-month recall, to continue his improvement.
EVALUATION:
The patient was very excited to incorporate an electric toothbrush into his daily oral hygiene routine. On the last visit he told me that he bought the Oral-B electric brush. He finally started to enjoy cleaning his teeth more, because with an electric brush it was so much easier for him. I believe that it was very important to show the patient the calculus and plaque present in his mouth. At the conclusion of his visit, the patient understood that, with better flossing and brushing technique, he could more effectively remove plaque accumulation between his teeth.
At the patient’s first visit, the patient had moderate inflammation and bleeding upon probing, with pink, redness areas on cervical third and non-stippled gingiva, generally bulbous and firm. On his second visit, the patient presented reduced bleeding (from moderate to minimal) upon probing and reduced gingival inflammation. This indicates that his tissue became more resilient.