This category provides patient cases that have challenged and expanded my clinical skills in patient management as well as instrumentation.
CASE I
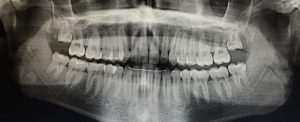
This first case may seem rather simple, but challenged my clinical skills even more than heavy cases with periodontal involvement. Case I illustrates the before and after of a patient with a fixed lingual retainer. This was my first experience involving a fixed lingual retainer and my calculus removal was compromised because of my timid motions. The patient is a 20 year old male who hadn’t received an oral hygiene visit since the removal of his braces in 2015 and was not using any inter-dental aid. Home care instructions were the most critical part of the visit and flossing with GUM soft picks was demonstrated as traditional floss was uncomfortable for the patient. A panoramic and 4 horizontal bite wings were taken during the visit as one caries was detected clinically and third molars were partially erupt. Though this patient was a medium case value and a type I periodontal value, dietary habits of frequent carbohydrate exposure and sticky candy with the lack of skill in maintaining a fixed lingual bar calls for a 3 month recall until build up is well controlled.
CASE II
This case involves a patient I’ve treated since my first semester in the program and shows tremendous growth in patient implementation with initiative to change poor oral habits and achieve optimal oral hygiene instructions. Though there are no pictures provided for this case, plaque scores continued to decrease, calculus detection brought the case value from a heavy to a light from (2015-2017) and patient habits aimed for maintenance of incipient caries lesions while patient goals were always achieved by the recall appointment. During the first appointment in 2015, digital x-rays revealed calculus in all quadrants and inter-proximal buildup was heavy, clickable and generalized on all posterior surfaces. In short, this patient was a perfect candidate for the boards when assessments were completed during the initial visit. The patient was not flossing and began to use Glide Floss Picks three times a week. During his recall appointment, the patient was flossing five times a week and by the last visit under my care, he was flossing once a day. With clinical caries detected and a caries risk form completed, the patient was placed at a high cares risk and started using Listerine Total 10 mL (2 teaspoonfuls) for one 1 minute and 1.1% NaF toothpaste 2x day.
CASE III
This particular case involves a 24 year old male who never had a dental appointment or oral hygiene visit primarily due to dental anxiety. During EOIO, the patient had a nodular protrusion approximately 2×2 inches around the occipital region of his head. The lesion was alarming because of the firm texture at the center and generalize inflammation. The patient stated that it has been present for 10 years due to trauma with a razor yet mentioned the size had increased over the last few years. A referral was given to a general physician and dermatologist for further observation. Regardless of no previous dental visit, the patient was classified as a light and perio type I, however, a full mouth series was exposed as a guideline and necessary due to two deciduous molars remaining in the dentition. The full mouth series revealed impacted permanent second premolars on the maxilla. The patient was advised to followup with a PA of the region every few years or seek special treatment from an oral surgeon if pain were to start at any point of his life. Clinically, no bumps were felt around the gingiva and the patient did not experience any pain in the area throughout his life. A referral and a copy of the x-rays were released to the patient in the event that he may experience any pain or choose to undergo any orthodontic treatment.
CASE IV
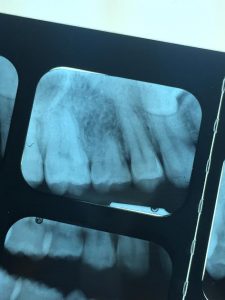
The last case I will share with you is regarding patient management and change that may correlate to pathology that was detected. The patient is a 76 year old female taking Metformin as an anti-diabetic medication once a day. Her blood pressure during her morning appointment was within normal limits and well controlled. During assessments, mobility of #2 was detected and #20-DF was being monitored for a deep pocket reading of 7mm at the prior visit (3 months earlier). During periodontal charting, #20-DF measured 11mm. The patient had generalized 4-6mm readings, generalized 1-2mm recession and the clinical attachment loss ranged from 4-8mm, classifying her as a perio type III. Since this deep pocket had increased so drastically a FMS was taken. The patient had been seen in our clinic since 2005 and the last films exposed were 4 VBW in 2014. The patient had never received a full mouth series. Films revealed pathology around the apex of #20, relative to the deep pocket measurement. A referral was given to further examine the findings to determine the next course of action. The x-rays also revealed a caries on #4-D and a referral was also given to a DDS as well as #2 mobility to be evaluated. Aside from the findings of this visit, a positive update was the case value reduction from a medium to a light and calculus on lower anteriors was minimal as the patient continued to use the GUM floss picks with a larger diameter.
Vertical Bite Wing taken in 2014
Updated film in 2017 of the same location