Patient is a 69 year old Caucasian Female
Chief Concern
Patient stated that they are here for a cleaning.
Medical Hx
Patient reports being diagnosed with asthma, psoriatic arthritis, high cholesterol, seasonal allergies, osteoporosis, and hypertension. Patients’ last medical exam was 3 months prior. Patient was hospitalized 7 months prior for a fractured right hip. She received a full hip replacement and was hospitalized for 1 week. Physician reported that she did not need pre-medication for dental cleaning. Patient has not had an asthma attack in over a year. Patient is allergic to Enbrel, had reaction to injection. Medications include Prolia 1 injection every 3 months for osteoporosis, apremilast 30 mg 2x/daily for psoriatic arthritis, budesonide 2 puffs in the morning and singulair 10mg in the evening for asthma, fluticasone nasal spray 1x/daily for seasonal allergies, simvastatin 40mg 1x/daily for hyperlipidemia. OTC meds include 1 baby aspirin daily. Vitamins include folic acid 1mg 1x/daily. Patient is ASA 2 based on conditions and allergies.
Social Hx
Patient reports no tobacco or recreational drug use. Patient has 1 glass of wine with dinner every night.
Dental Hx
According to the patient, the last dental examination was about 9 months prior where she had a PAN done and implant placed. Last cleaning was at NYCCT 1 year prior. Patient reports using Oral-B electric toothbrush at night and a manual toothbrush before and after breakfast. She flosses 1x/daily with traditional floss and uses Listerine 1x/daily.
Vitals
Blood pressure was 124/85 which corresponds to stage 1 hypertension. Her pulse was 69 BPM.
Assessment
Head and Neck Exam
- Extra-oral: Asymptomatic crepitus on the left TMJ.
- Intra-oral: Asymptomatic enlarged nodule on the left labial mucosa, adjacent to commissure. Traumatic lesion 1mm in diameter on the right labial mucosa adjacent to commissure, 1mm red macule on the right soft palate, 2 red/purple macules on the right buccal mucosa, bilateral linea alba.
Dental charting
Localized abfraction on #3-5 and #12-14. Class of occlusion: bilateral class I. Overbite 30%. Overjet 2mm. #29 is missing restoration (pt. was not aware).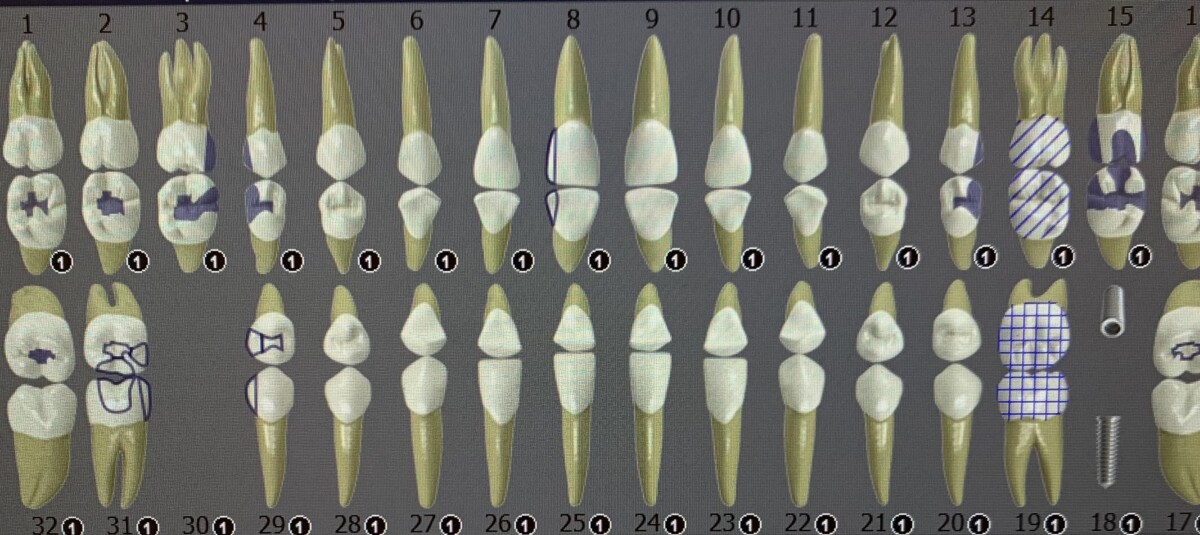
Periodontal Assessment
Generalized pink, firm, smooth gingiva with rolling at the gingival margin. Gingival margin is apical to CEJ from recession.
Generalized 1-3mm pocket depths with minimal BOP, localized 4mm pocket depths on molars, localized 3-8mm CAL on premolars. Implant was not probed because it was not fully healed.
Stage II Grade B Periodontitis
Caries Risk
Moderate risk based on CAMBRA.
- Patient was encouraged to continue self reported hygiene routine, but encouraged to incorporate a water flosser because it effectively removes food particles and debris from hard-to-reach areas around the implant and restoration margins, reducing the risk of plaque buildup, bacterial growth, and inflammation, thus promoting the long-term success and stability of the dental work. Additionally, she was also encouraged to use fluoridated oral rinse for caries prevention.
Calculus Detection
Case value: Medium
Generalized moderate subgingival calculus and moderate supragingival calculus.
Treatment
Patient was completed in one visit. Medical hx, dental charting, perio charting, and calculus detection were completed. Scaling and root planing was performed on the entire mouth with ultrasonic and hand instruments, engine polishing was performed, and sodium fluoride 5% was applied. Patient was given a referral for blood pressure to be evaluated. She was also given a referral for her missing restoration on #29 to be evaluated. Patient was given a 3 month recare based on periodontal status.


