Patient is a 60 year old African American Female
Chief Concern
Patient stated they needed a dental examination and cleaning.
Medical Hx
Patient reports being diagnosed with type 2 diabetes and hypertension. She is under a physicians care, and her last physical was two months prior. At that appointment her HbA1C was 5%. She reports eating before the appointment. Patient has no allergies. Patient takes sitagliptin (Januvia) 40mg 1x/daily for diabetes, amlodipine 25mg 1x/daily for hypertension for about three years and she reported taking them before the appointment. Patient is ASA 2 because of well controlled diabetes and hypertension.
- Inquiring about regular care from a physician is essential for patients managing both high blood pressure and diabetes, ensuring comprehensive health management and coordination between dental and medical treatments to optimize overall well-being.
- It is crucial to request the most current HbA1c levels of diabetic patients undergoing dental cleaning to mitigate potential complications associated with fluctuating blood sugar levels.
- It is important to inquire whether a diabetic patient has eaten before their appointment to gauge their current blood sugar levels accurately, preventing potential complications related to hypoglycemia or hyperglycemia during treatment.
- It is beneficial to research the medications patients are taking to assess potential side effects that could negatively impact their oral health. It also enhances the clinician’s overall knowledge of medications.
- It is vital to inquire about the patient’s compliance with their medications on the day of the appointment as it can significantly impact treatment outcomes and patient safety.
Social Hx
Patient reports no alcohol, tobacco or recreational drug use
Dental Hx
Last dental examination and cleaning was 9 months prior. Last radiographs were taken over 5 years ago. Patient reports no pain or sensitivity. Patient reports using manual and Oral-B electric toothbrush after every meal, flosses 2x/daily with traditional floss and uses Listerine oral rinse 2x/daily. She reports having more plaque buildup since taking medications.
Vitals
Blood pressure was 151/91 and pulse was 88 on the first reading, the second reading was done five minutes later and it was 146/95, and the third reading was done an hour later and it was 158/96. This corresponds to stage 2 hypertension. Patient was able to continue with non-invasive treatment but was instructed to provide medical clearance from her physician for next appointment. Patient was compliant and returned with clearance. Blood pressure was ….
Assessment
Head and Neck Exam
- Extra-oral: Small, moveable nodule on left cervical chain with no pain on palpation. Small moveable nodule on the right sublingual gland with no pain on palpation.
- Intra-oral: 1 mm in diameter, red macule on right and left buccal mucosa from cheek biting. 2mm in diameter amalgam tattoo on floor of mouth, right of the midline.
Dental Charting
Class of occlusion: Class II right, class I left. Overjet: 0mm. Overbite 0%.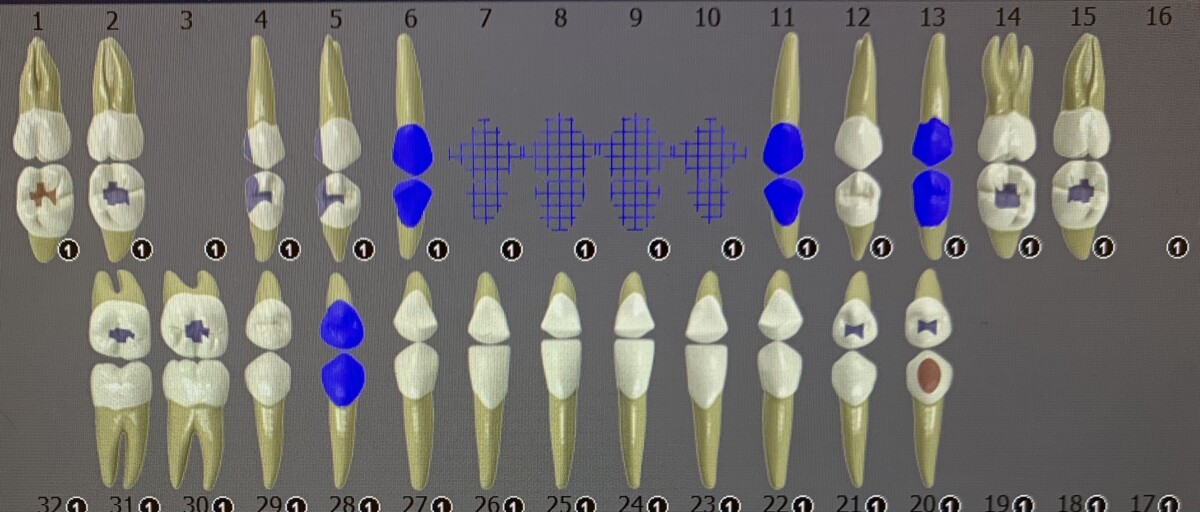
Periodontal Assessment
Generalized red, shiny, soft gingiva with rolling at the gingival margin and slightly bulbous papilla. Gingival margin is apical to CEJ from recession.
Generalized 1-4mm pocket depths with BOP.
Stage IV Grade B periodontitis based on FMS.
Caries Risk
High based on CAMBRA. Patient was told to drink an adequate amount of water and start the use of Biotene to counteract the xerostomia caused by medication. She was also told to be consistent with oral hygiene by receiving a cleaning every three months.
Calculus Detection
Case Value: Heavy
Generalized heavy subgingival calculus and generalized moderate supragingival calculus concentrated to the lingual surfaces of the mandibular anteriors.
Treatment
Patient was completed in two visits. In the first visit; medical history, head and neck exam, dental charting and a FMS were completed. Taking a FMS on a patient who has not had x-rays in over 5 years, is diabetic, and suffers from xerostomia is necessary to assess for potential carious lesions and/or bone loss. Oral home care instructions were given to continue with the use of electric toothbrush, traditional floss. She was also encouraged to use Biotene 1 x/daily to alleviate the symptoms of xerostomia induced by her medications. On the next visit, the patient returned with medical clearance; perio charting, and calculus detection were completed. Scaling and root planing were performed on the entire mouth with ultrasonic and hand instruments, engine polished, and sodium fluoride varnish 5% was applied. Patient was given a referral for blood pressure and suspected carious lesions. Patient was given a 3 month recare based on their periodontal status, xerostomia, and diabetes.


