Case Study #1
Mr. KC is a 36-year-old Hispanic male and presents with braces, extrinsic black line staining, and gingival inflammation. A full medical intake and a full dental examination were performed. Mr. KC was an ASA 1 and hadn’t seen a dentist since he had placed his braces 5 years ago, in his home country. He had mentioned to me that some of his brackets had broken off and he needs an orthodontist. Mr. KC also had a few areas of suspicious decay noted on tooth #1, 2, 31, 32; a referral and list of local dental facilities were given to the patient.
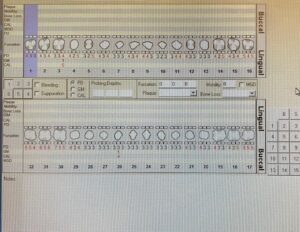 Being that Mr. KC had braces it was difficult to probe the buccal’s of his dentition, therefore probing was only obtained on the linguals. Perio readings ranged from 3-7mm, generalized. The patient also had significant inflammation with type two embrasures with loss of stippling and BOP. We diagnosed the patient as a medium, generalized gingivitis, and the rationale behind this diagnosis because we could not take x-rays to verify the crestal bone and if there is any presence of bone loss.
Being that Mr. KC had braces it was difficult to probe the buccal’s of his dentition, therefore probing was only obtained on the linguals. Perio readings ranged from 3-7mm, generalized. The patient also had significant inflammation with type two embrasures with loss of stippling and BOP. We diagnosed the patient as a medium, generalized gingivitis, and the rationale behind this diagnosis because we could not take x-rays to verify the crestal bone and if there is any presence of bone loss.
Mr. KC did not floss his teeth but brushed and used an oral rinse 2x a day. He found flossing too hard to do with his braces. I introduced him to the floss threader and he understood the concept but he said that he would not be able to do it every day. I contemplated what would be best for my patient time-wise and healthwise and I decided that soft picks would be best in his situation.
Mr. KC’s treatment was split into two visits: The first visit was a full debridement of quadrants 1 and 4 and the following visit we completed treatment. I gently scaled around his brackets and on the linguals of 6-11 to remove all of the stains that have accumulated over the years. Lastly, I engine polishing with a paste mixture of pumice, hydrogen peroxide, and water to remove any black line stains that I was unable to remove with my Nevi, and 5% Na fluoride was applied.
Case study #2
Mr. MM is a 29-year-old Hispanic male with a BP of 137/77, this is considered hypertension stage 1, and Mr. MM is considered an ASA 2. Mr. MM had not been to the dentist in over 10 years. A full medical intake and a full dental examination were performed on Mr. MM. An oral cancer screening was performed and Mr. MM was told the importance of this and he was informed of statistics about oral cancer. I found bilateral linea alba that extended into the commissures, a fissured tongue, and swollen left sublingual caruncle, about 3×3 mm. Suspicious Upon palpations, it was hard and movable; The patient was asymptomatic. The patient was approved for a panoramic x-ray. On the pan, you can see a radiopacity adjacent tooth #24/25. Mr.MM was given a referral for suspicious caries and the lesion of the sublingual gland. 
Mr. MM had very visible generalized supragingival calculus deposits, as well as super tenacious subgingival deposits. His periodontal status is classified as Stage 1 grade B; probing depths ranging from 3-8mm, with significant BOP.
Scaling Mr. MM would very difficult being that the calculus was very tenacious. His treatment was divided into three visits. I started treatment on Mr. MM ( full debridement of quadrant #1 and his treatment was completed by another provider, due to conflicting schedules.)
I followed up with Mr. MM a few days after I saw him, I inquired if he has seen an oral surgeon to address the intraoral findings of the sublingual gland. He had told me that he was out of town and would follow up once he returned. I told him I would like for him to go as soon as he returns, and the importance of why. Mr. MM has since been non-compliant regarding this issue.













