In February, I had a new patient (44 yr old Filipino male) who stated his last hygiene services were over 10 years ago. He had a full physical about 4 weeks before he came into the clinic. His daily medications are as follows:
Metformin, 2000mg/day (Type 2 Diabetes); Trulicity, 1.5mg/day (Type 2 Diabetes); Rosuvastatin, 10mg/day (high cholesterol); Daily Supplements: Multivitamin, Elderberry
In addition to his Diabetes and high cholesterol, he was found to be in Stage 2 hypertension when I took his vitals. First reading – 148/98, pulse 76. Second reading – 146/99, pulse 83. When I asked him if he had a conversation with his doctor about his BP readings at his last physical, he stated it has never been an issue and his physician has not recommended BP medication. His HbA1c at this appointment was also an astounding 7.9! To my further dismay, he revealed he does not have an at-home blood glucose monitor. He stated he has never been told he needed one. He admitted to having a particularly poor diet recently due to stress, pandemic and otherwise. He also drinks socially and smokes marijuana about once per week.
His oral hygiene routine consists of using a Sonicare electric toothbrush twice per day, but no regular flossing.
Knowing the bi-directional relationship between periodontal disease and diabetes I decided, along with my instructor’s approval, that he should not be turned away. A full debridement would only serve to improve his overall health. Although he had eaten a balanced breakfast that morning, I obtained something from the vending machine to have close by should his blood sugar fall during his time in the chair.
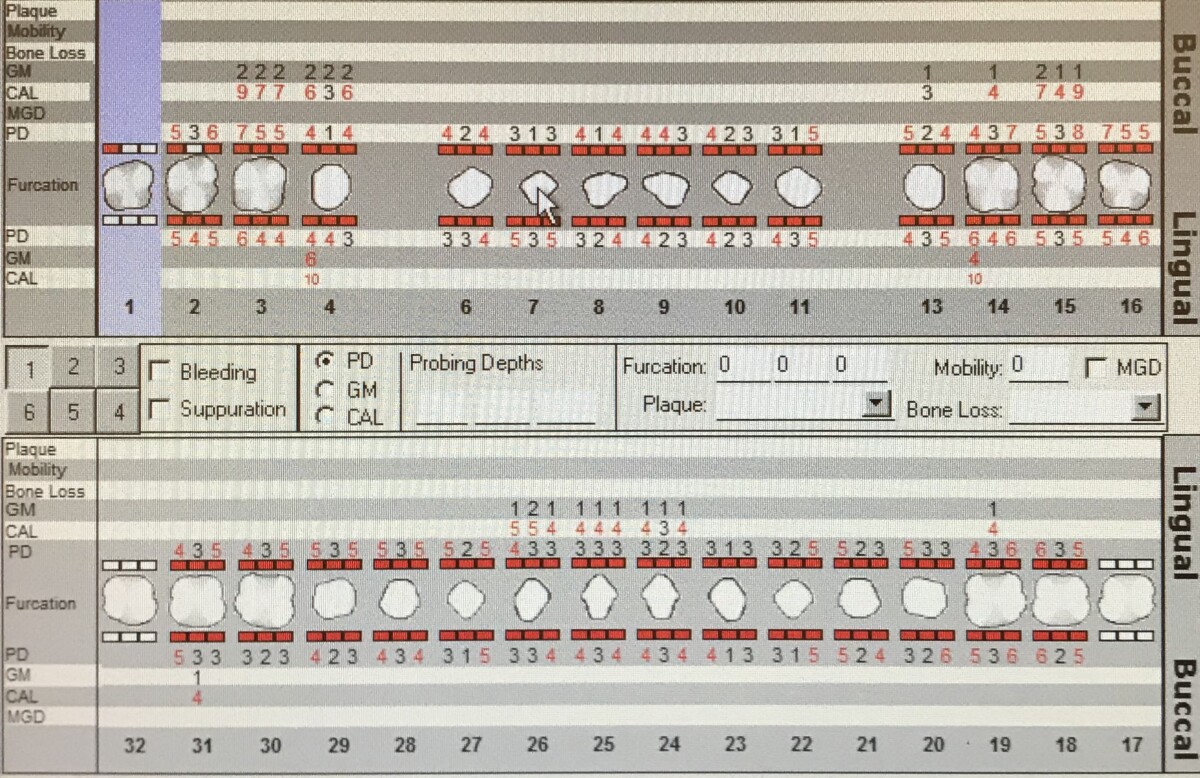
His assessments revealed severe generalized inflammation, with rolled margins, bulbous papillae, and heavy BOP. He had had supra- and subgingival calculus. His probing depths and recession are to follow:
It was also in good judgement, after seeing the state of his oral health clinically, to expose a full mouth series of radiographs to give us a baseline and be made aware of possible pathologies. The radiographs below revealed periapical radiolucencies around #s 3 and 4, caries present on #s 13 and 14, and also the extent of coronal breakage/decay on #19 (previous RCT) and #32. There is also radiographic evidence of bone loss and subgingival calculus.
Based on his assessments, he is a Periodontitis Stage II, Grade C when considering bone loss, probing depths, and diabetes. I made his treatment plan for 2 more visits, scaling quadrants 1 and 4 on the first visit, and quadrants 2 and 3 during the second. For pain management, the patient agreed to try Oraquix. I gave him a referral for the pathologies mentioned above, as well as a separate referral for a consult regarding his elevated blood pressure. I educated him on the importance of a thorough oral hygiene routine and how it can affect his diabetes, and vice versa. I strongly encouraged him to monitor his blood glucose on his own, so he can better manage his condition.
The first day of his cleaning, I introduced flossing technique and he revealed he had never been shown the proper way to floss in the past. There were only 2 days between cleaning the right side and the left side, but there was already noticeable improvement. His blood pressure on that day of his last appointment was also much more satisfactory – 122/88, pulse 82! He stated he did not drink as much coffee and drank more water that morning. It is possible he also had less anxiety as he now knew what to expect regarding treatment. There were currently embrasures present in the anterior due to tissue shrinkage, as he responded well to previous hand-scaling with Oraquix. I proceeded with cleaning the left side, quadrants 2 and 3, while avoiding the unstable teeth #s 13, 14, and 19. Upon completion, I placed him on a 3-month recare schedule and reiterated the two-way relationship between diabetes and periodontal disease. I encouraged him once again to monitor his glucose at home and to incorporate proper flossing into his daily routine.