Case Study 1: Penicillin, Implant Maintenance
Initial Visit:
The patient under examination was a 44-year-old Asian male. The patient’s initial blood pressure was 127/90 (corresponds to HBP Stage II) Pulse. After providing the patient water and some time to relax, after 5 minutes passed, we retook their blood pressure and it was BP: 123/87 (corresponds to HBP Stage I) Pulse 95. The patient reported that they have a penicillin allergy and are lactose intolerant, when consumed they experience gastrointestinal symptoms. The patient takes one daily dose of a nature-made multivitamin and ibuprofen as needed. The patient was examined medically on March 1, 2019, and on March 21, 2022, they underwent a dental examination that included a cleaning, four radiographic images, and a PANO exposure. The patient reported that they had implants placed five years ago. They had implant and periodontal maintenance in Tijuana, Mexico as part of their dental exam. In addition, the patient reported regular consumption of three servings of alcohol per week and daily usage of e-cigarettes (previously used traditional cigarettes, a decade ago) for about 30 years. The patient’s oral hygiene regimen at home consists of utilizing floss picks three times a day in addition to an Oral B electric toothbrush with Listerine and Colgate Whitening twice a day.
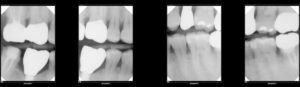
After conducting a comprehensive examination, it was revealed that the patient presented with multiple restorations with filings, implants, and porcelain crowns along with a gingival graft on #8 (facial aspect). The patient presented with generalized red-pink bulbous marginal gingiva which is more evident on the anteriors, with rolled smooth, shiny, irregular marginal gingiva due to receded areas, and generalized bleeding upon probing. A vertical bitewing series was performed which revealed a periodontal classification, Heavy Stage III Grade B due to generalized horizontal bone loss of more than 15%, smoking habits, and CAL. The patient was provided a referral for evaluation of a carious lesion seen on the VBW on #4 (M).
The patient’s treatment plan consisted of two visits which included the initial visit. We began providing oral hygiene instructions and we focused on teaching Modified Bass Technique as the plaque index score that we conducted was 1.3, a fair range, and the biofilm mainly appeared on the direct buccal and lingual aspect of the tooth and interproximally. After education was discussed and demonstrated, the patient was for pain management so we started with Oraqix on Q1. Q1 was scaled using cavitron tip and hand-scaled.
Revisit #1:
During the revisit, we retook the patient’s BP and it was 110/84 (corresponds to HBP Stage I) Pulse 90. Upon re-examination of the area scaled, the patient presented with generalized light pink marginal gingiva that still had areas of marginal redness on the lingual aspect. There were no significant changes since the last visit and the patient reported that they have attempted to incorporate the Modified Bass Technique every night. The plaque score was not changed and the spool method was demonstrated. The patient felt comfortable with the technique and reported that they will attempt to use it in their daily routine. Administration of 20% topical benzocaine on Q2, 3, and 4. Administration of two carpules 1.7 carbocaine, mandibular right mental block, and long buccal was given. The patient reported that the anesthesia had worn off and requested a longer dosage. Faculty administered left-side alveolar block and longa buccal and mental block. Along with AMSA, PSA maxillary left quadrant, infiltrations with carbocaine 0.4 carpule 1.7 cc. Scaled Q2, 3, 4 using cavitron tip and hand-scaled. Engine Polished. Application of 5% Fluoride Varnish was placed. The patient was recommended to come back for a 3-month recall.