CASE 1:
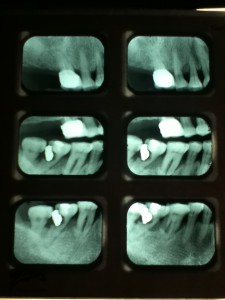


69 year-old Asian female, non-smoker, no history of systemic diseases, diagnosed with osteoporosis about eight years ago. Patient presented with heavy calculus and staining. She was classified as heavy type III periodontitis and has generalized probing pocket depth 5-6mm, localized area of 7mm, moderate BUP. Her gingiva appeared to be red and swollen. Gingival margin exhibited rolled or rounded shape with blunted and bulbous interdental papillae. Upon taking a full mouth series of x-ray, generalized horizontal bone resoprtion of 3mm or more was noted, and localized vertical bone resoprtion and decay were observed as well. The radiographs were consistent with clinical findings. During review of home care, patient stated that she had never flossed and rinsed, and brushed twice a day. So meticulous oral hygiene instructions were given.
The treatment plan consisted of a total of four visits. The 1st visit was complete assessment and scaling and root planning of LR quad. The 2nd visit was scaling and root planning of UR quad. A referral for caries and perio evaluation was given to patient. The 3rd visit was scaling and root planning of UL and LL quads, and patient was placed on a 3 month recall. The 4th visit was place ment of Arestin. When patient returned 4 weeks after placement of Arestin, both she and I were very impressed with the outcome. Her gingiva was less inflammed and bleeding reduced. The probe reading went down 1-2mm in the area where Arestin was placed. Overall, the case was a success.
Below is comparison of probing depth between pre-Arestin and post-Arestin:
Tooth number & surface |
Initial probe readings |
Post-Arestin readings |
| #3MB | 5mm | 4mm |
| #5MB | 5mm | 5mm |
| #6MB | 5mm | 5mm |
| #7DB | 5mm | 5mm |
| #12MB | 5mm | 4mm |
| #12DL | 5mm | 4mm |
| #13DB | 5mm | 4mm |
| #22ML | 7mm | 5mm |
CASE 2:
62 year-old African-American female, non-smoker, has no history of systemic diseases. The patient was classified as Medium/Type II. Patient has generalized pocket depth 4-5mm, localized 6-7mm, and generalized gingival recession. Her mandibular anterior teeth presented with slight to moderate mobility. Upon taking a full mouth series of x-rays, periapical cemental dysplasia was clearly observed on mandibular anterior teeth. A referral to see oral surgeon for evaluation was given to patient.
CASE 3:
43 year-old African-American male, smoker, has no history of systemic diseases. Patient stated that he has not had his teeth cleaned for ten years. During review of home care, patient stated that he had never flossed and rinsed, but brushed twice a day. So meticulous oral hygiene instructions were given. Patient presented with heavy subgingival calculus on entire mouth and heavy supragingival calculus on mandibular anterior teeth. Comparison between pre-scaling and post-scaling is displayed as follows:
Before scaling: After scaling:
Pieces of calculus removed from mandibular anterior teeth
CASE 4:
The photos were taken on April 28, 2015 on my clinic patient, 32-year-old Asian female. The patient presented with moderate stain on mandibular anterior teeth. Prophyjet was utilized to remove those stain. Comparison is shown as follows:
Before using prophyjet, stains on mandibular anterior teeth was clearly observed.
After using prophyjet, stain was removed.
CASE 5:
The photos were taken on March 31, 2015 on a clinic patient. My classmate and I successfully used the prophyjet to remove the patient’s supra gingival stain from lingual and facial surfaces of his mandibular anterior teeth. Comparison is shown as follows:
Before using prophyjet
After using prophyjet














