Introduction
For my Community Nursing, clinical I was working alongside RN preceptor Nuri Beltre at Woodhull Medical and Mental Health Center (Medicine Practice Group A Clinic), 760 Broadway, Brooklyn, NY 11206. Wednesdays, from 8:30 am – 12:40 pm.
Our team service learning project involved diabetes education for the community. Diabetes is prevalent diagnosis within this community, and it was important to address this issue.
Our goals and objectives of the service learning project included:
1) Acknowledge unique cultural perceptions of health and provide clients with a better understanding of the disease processes of diabetes
2) Educate and assist clients to manage diabetes through combined interventions such as behavioral modifications, dietary improvements, increased physical activity, and closely monitored medication regiments.
3) Ensure clients have a thorough knowledge of the diagnostic tests to monitor diabetes progression in the short-term efforts to lower blood glucose levels, while long-term goals are centered on mitigating further complications, morbidity, and premature mortality associated with the condition.
4) Identify strategies to maintain normal blood glucose levels
5) Address selected barriers that stem from social determinants, such as, culturally adapted interventions, community health workers, and financial assistance for clinical treatment and behavioral changes.
6) Address intervention limitations due to physical and social factors, such as low income, employment insecurity, low educational attainment, and poor living conditions, and how all of the above can affect behavioral modification.
Objective 1: Demonstrates individual professionalism through personal behaviors and appearance.
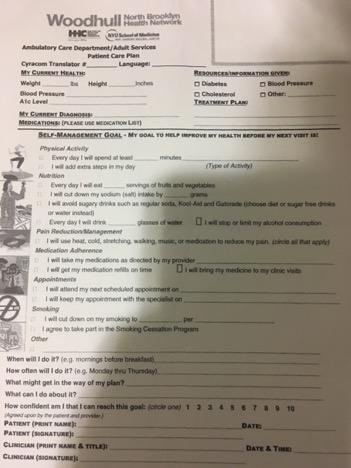
For my community clinical in Woodhull Medical Clinic myself and RN Beltre screen new patients and provide follow up nursing visits for the preexisting clients. Each client is seen individually in the privacy of an exam room at the clinic. When we screen clients for RN visit we do a detailed questioner and nursing care plan which is patient centered. We work with the client and tailor the care plan to his or her individual needs. If there are discrepancies that need to be addressed, we contact the provider MD/NP with collaborative care and teamwork to make certain the patient receives the appropriate treatment and care plan.
In addition, I attend weekly meetings with nursing leadership staff, MD/NP providers, and all the staff nurses. During these meetings data and statistics are discussed in terms of Quality Improvement (QI). Last week data was presented that Woodhull Medical Clinic is under performing with optimal diabetes care being 28.9%, hypertension control being 69.5%, depression treatment 32.9% and since we are in valued based care as per CMS, the providers were concerned that they will lose CMS funding if the statistics do not improve. (Woodhull NYC Health and Hospitals, 2017).
As always the dress code is processional business attire with an identification clearly visible for the hospital staff and the clients that we screen.
Objective 2: Employ analytical reasoning and critical thinking skills when providing care to individuals and families in the community setting.
Before the client is seen at the clinic we pull up his or her computer record. If this client been at the clinic before, we are able to assess pertinent information such as past medical history, medications, labs, last visit, immunizations etc. If this the first visit by the client than we will not find any information in the computer. Clients are also given PATIENT HEALTH QUESTIONNAIRE-9 (PHQ 9) which assess clients’ depression severity which was developed by Drs. Robert L. Spitzer, Janet B.W. Williams, Kurt Kroenke and colleagues. Myself and my Preceptor RN Belte go over PHQ-9 with the client to see if they understood the questions and if they are depressed and how severe is their depression to make appropriate referrals for collaborative care. If the clients are Hispanic and only speak Spanish, then RN Beltre speaks with them in Spanish so they can understand the information in their native language.
Objective 3: Effectively communicate with diverse groups and disciplines using a variety of strategies regarding the health needs of individuals and families in the community setting.
During clinical setting, myself and my preceptor communicate with the clients who come for nursing visits. If they are Spanish speakers, then my preceptor will translate. In addition, our group build a community education project where we outlined nutrition education for diabetic clients. In the Geriatric clinic, we presented our project to the clients. We the help of Estefani our group member, she was able to deliver nutrition information to diabetic clients in Spanish.
Objective 4: Establish environment conducive to learning and use a plan for learners based on evidence-based practice.
When the clients first come to a clinic nursing visit, it’s important to assess the client as an individual. To ask the client what is it that we can help him or her with. It’s important to note it’s what client wants and not what myself want for the client. After listening to the client and the reason he or she is seeing care, we then obtain the necessary physical findings, such as vital sings, physician exam etc. After the client goes to see the provider MD/NP. After there is care plan/teaching plan that is established with clients input and listening to what is important to the client.
Before the client leaves the clinic he or she will verbalize back the teaching and will co-sign the care plan acknowledging understanding and intent to follow.
Objective 5: Utilize informational technology when managing individual and families in the community.
During clinical setting, myself and my preceptor consistently assess clients records utilizing the computer. We will look up pertinent medical history, medications, recent visits, immunizations etc. All provider orders are also computer aided. Informational technology if used properly can be a very effective tool to improve patient safety and quality of care rendered. For instance bar-code technology can be used to reduce medication errors. A study by Poon and colleagues discovered that on units without the bar-code eMAR scanner “we observed 776 non-timing medication-administration errors (an 11.5% error rate), whereas on units with the bar-code eMAR, we observed 495 non-timing medication-administration errors (a 6.8% error rate), representing a 41.4% relative reduction in the rate of such errors. The rate of potential adverse drug events due to non-timing administration errors fell from 3.1% to 1.6%, representing a 50.8% relative reduction” (Poon, 2000, p.1698). Thus, in this instance Poon & colleagues were able to demonstrate evidenced based practice of bar-code technology on the safety of medication administration. In Woodhull clinic all vaccines are bar-code technology operated to avoid any errors.
Objective 6. Demonstrate a commitment to professional development
In my nursing NUR 3110 Leadership and Management course we all took courses from Institute for Healthcare Improvement with courses ranging from Health Care Improvement, Patient Safety, Leadership, Person-and Family-Centered Care, Improving Health Equality etc. (IHI, 2017). After completing these online module courses we received a Basic Certificate in Quality & Safety. Utilizing online module courses work we are utilizing competencies of Informatics, Evidenced-Based Practice EBP, and Safety.
For my community clinical in Woodhull Medical Clinic, I attend weekly meetings with nursing leadership staff, MD/NP providers, and all the staff nurses. During these meetings data and statistics are discussed in terms of Quality Improvement (QI). Last week data was presented that Woodhull Medical Clinic is under performing with optimal diabetes care being 28.9%, hypertension control being 69.5%, depression treatment 32.9% and since we are in valued based care as per CMS, the providers were concerned that they will lose CMS funding if the statistics do not improve. (Woodhull NYC Health and Hospitals, 2017).
During the clinical when we see patients for RN visits we do a detailed questioner and nursing care plan which is patient centered. We work with the client and tailor the care plan to his or her individual needs. If there are discreteness that need to be addressed, we contact the provider MD/NP with collaborative care and teamwork to make certain the patient receives the appropriate treatment and care plan.
Objective 7. Incorporate professional nursing standards and accountability into practice
Tenets Characteristic of Nursing Practice
- Nursing practice is individualized.
Nursing practice respects diversity and is individualized to meet the unique needs of the healthcare consumer or situation. (ANA, 2008)
- Nurses coordinate care by establishing partnerships.
The registered nurse establishes partnerships with persons, families, support systems, and other providers, utilizing in-person and electronic communications, to reach a shared goal of delivering health care. (ANA, 2008)
- Caring is central to the practice of the registered nurse.
Professional nursing promotes healing and health in a way that builds a relationship between nurse and patient.). (ANA, 2008)
- Registered nurses use the nursing process to plan and provide individualized care to their healthcare consumers.
Nurses use theoretical and evidence-based knowledge of human experiences and responses to collaborate with healthcare consumers to assess, diagnose, identify outcomes, plan, implement, and evaluate care. (ANA, 2008)
All the ANA tenets are incorporated in the care that we render to all the clients that visit the clinic. I hole headedly believe everyone who earns RN license is there for the client and to help alleviate pain and suffering. Caring is central to the practice of nursing!
Objective 8. Collaborate with clients, significant support persons and members of the health care team
During my NUR 4010 Community Health Nursing clinical I had a specific case where collaboration between Doctor, RN and myself saved someone from going to the E.R. in an unstable condition. This case started when Dr. Shapozhnikov the attending M.D. informed her to contact Ms. S. a patient that was seen in the clinic yesterday and have her come in immediately. Ms. Beltre explained that Ms. S came for her scheduled clinic appointment to check her sugar and diabetes medications prescriptions. In the clinic, her initial finger stick was 410mg/dl and Woodhull’s policy is to repeat the exam when a critical value is seen, and follow up finger stick was 426mg/dl. Ms. S was seen by an NP who made only slight adjustment in her Metformin medication and sent her home. Dr. Shapozhnikov was concerned that Ms. S needs further assessment, lab work, and medication adjustment that includes an insulin prescription and he wanted her to come back to the clinic immediately so that she can receive that care.
Ms. Beltre called Ms. S several times and left phone messages to call back the clinic urgently. However, as the day went by, we were losing hope that she would call back, thinking perhaps she went to the emergency room somewhere. Ms. Beltre tried calling one last time and Ms. S answered the phone. It turned out that she forgot to charge her phone and only now plugged it in and she was at home all day complaining about being very thirsty and urinating frequently. Ms Beltre explained to her that she needs to come in to the clinic and be seen by Dr. Shapozhnikov immediately. Ms. S agreed to come back to the clinic at 3pm.
Objective 9. Recognize the impact of economic, political, social and demographic forcesthat affect the delivery of health care services
Currently, health care in United States is operating under value based system. After each patient is seen by a health care provider in a hospital setting, the patient will get a survey in the mail called: Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey. This survey includes:
“1. Communication with nurses
- Pain management
- Timeliness of assistance
- Explanation of medications administered
- Communication with doctors
- Cleanliness of room and bathroom
- Discharge planning
- Noise level at night” (Manary, 2013, p.201).
If survey results come back poor consistently for a specific hospital, then said hospital does not get reimbursed for the care rendered. Centers for Medicare & Medicaid Services CMS in 2016 published Roadmap for Implementing Value Driven Healthcare in the Traditional Medicare Fee-for-Service Program. In said document CMS outlined very important measures and stipulations on reimbursement. If a hospital fails to provide care that the patients deems appropriate than federal reimbursement is withheld until they get fix their problems.
What clients want is to be to be heard by the healthcare team, informed of the team members taking care of them and be included in their plan of care. Emory Saint Joseph’s Hospital has implemented SIBR (structured interdisciplinary bedside rounding) program in their Accountable Care units, which “involves a collaborative health care team meeting with patients in their rooms to discuss their daily plan of care.” (Spence, 2015, para.1). During each individual SIBR visits, which lasts 4-6 minutes, the physician introduces the client to all team members and involves the client in a discussion about their care. Each team member comes to rounds “prepared to discuss areas of concentration such as overnight events, the patient’s goal for the day, nurse’s concerns, vital signs, pain control, intake, output, mobility, medication management and discharge plans.” (Spence, 2015, para.3). In Emory Saint Joseph’s Hospital model, we see direct patient input directed toward his/her care. The client is now in the driver’s seat and can discuss his/her concerns, wishes, and preferences directly with the team. Thus, communication/explanation is listed in 3 places in HCAHPS scores. After “Emory Saint Joseph’s Hospital in Atlanta began holding interdisciplinary rounds at the bedside and encouraging patients and family members to participate, length of stay dropped, patient satisfaction increased, and patient safety issues decreased on the units where the pilot was implemented.” (Making Patients Part of the Team Helps Hospital Cut LOS, Boost HCAHPS Scores, 2017, p.34). In addition, “the average score on the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) increased 16 points from fiscal 2015 to fiscal 2016 on the units” (Making Patients Part of the Team Helps Hospital Cut LOS, Boost HCAHPS Scores, 2017, p.35). Thus, having direct patient and family input in their care will improve patient satisfaction outcomes.
References:
American Nurses Association. (2008). Tenets Characteristic of Nursing Practice. Silver Spring, MD : Author.
IHI. (n.d.). IHI Home Page. Retrieved April 30, 2017, from http://www.ihi.org/Pages/default.aspx
Making Patients Part of the Team Helps Hospital Cut LOS, Boost HCAHPS Scores. (2017). Hospital Case Management, 25(3), 34-35.
Manary, M. P. (january 17, 2013). The Patient Experience and Health Outcomes. The New England Journal of Medicine ,3(368), 201-203. Retrieved May 5, 2017, from http://www.nejm.org/doi/pdf/10.1056/NEJMp1211775
Poon, E. G. (2010). Effect of Bar-Code Technology on the Safety of Medication Administration. The New England Journal of Medicine,362(18), 1698-1707. Retrieved May 2, 2017, from http://www.nejm.org/doi/pdf/10.1056/NEJMsa0907115
Spence, M. B. (2015, March 30). Emory Saint Joseph’s introduces new model of patient care. Retrieved May 05, 2017, from http://news.emory.edu/stories/2015/03/saint_josephs_SIBR/
Woodhull NYC Health and Hospitals. (2017). Population Health Dashboard [Brochure]. Brooklyn, NY: Author.