Patient Profile
The patient, a 33-year-old Caucasian female, presents with the main complaint of bleeding gums, and yellowing teeth in need of cleaning.
According to medical history, the patient states that she has Hepatitis C and received treatment for a month in 2019. The patient reported that she has no allergies, and she does not consume alcohol, drugs, or tobacco. The patient weighs 230 lbs and height 5’9”, with a BMI 34.
Vitals: BP reading is 119/78, and Pulse is 74, corresponding to normal. ASA-2 (due to History of Hepatitis C and excessive weight BMI -34).
Dental history: The patient reports using a soft bristle manual toothbrush in a vertical and horizontal motion 1-2 times a day using Colgate Total toothpaste. The patient uses floss 2-3 times a week and Listerine mouthwash 2-3 times a week. The patient doesn’t clean her tongue.
Clinical Findings
Extraoral findings revealed on the skin of the neck scarred length – 8 cm as a result of a burn at age 2. On the skin with the right side under the vermillion border, there is a residual scar/mark from a previous lip piercing.
Intraoral findings: Bilateral line Alba. The dorsal surface of the tongue has a white coating and is grooved in the midline of the tongue.
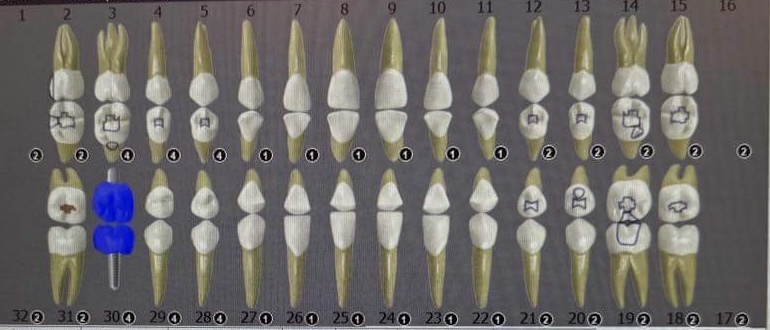
Dental charting indicated bilateral occlusion Class-1, Overjet-4mm, Overbite-20%. Caries activity: teeth #2-O, 15-O, 18-O, 31-O. Implant tooth #30. Teeth missing due to complications of caries: #1, 16, 17, 30, 32. The patient is at a high risk for caries.
Radiographic findings after exposed PAN, HBWs, and VBWs reveal a horizontal bone loss of 10% was noted. No periapical or jaw bone abnormalities were noted. There were no interproximal caries. Generalized interproximal calculus is present.

Before treatment

After treatment.
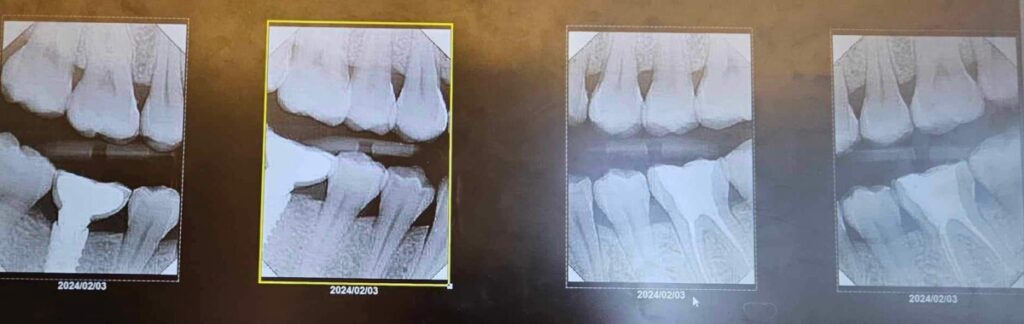
Bite wings images.
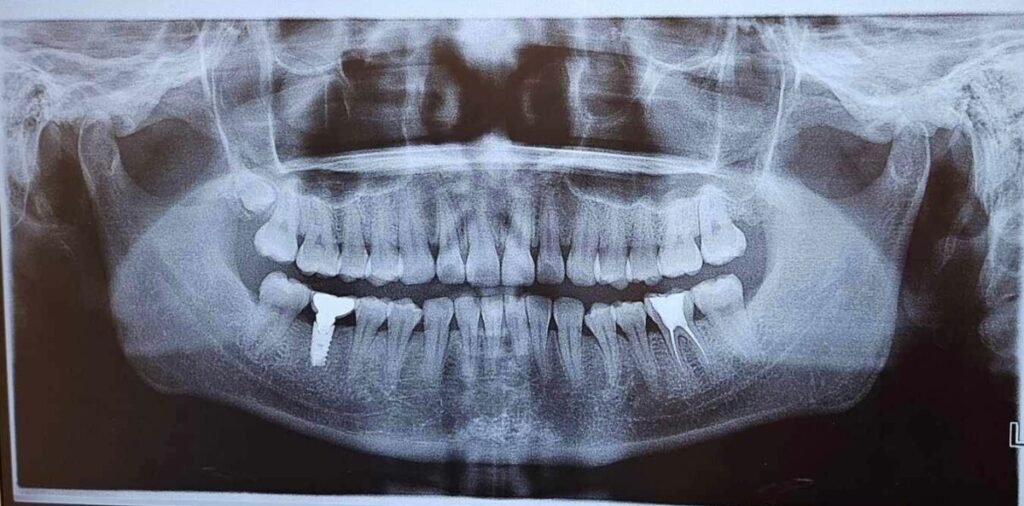
Panoramic image.
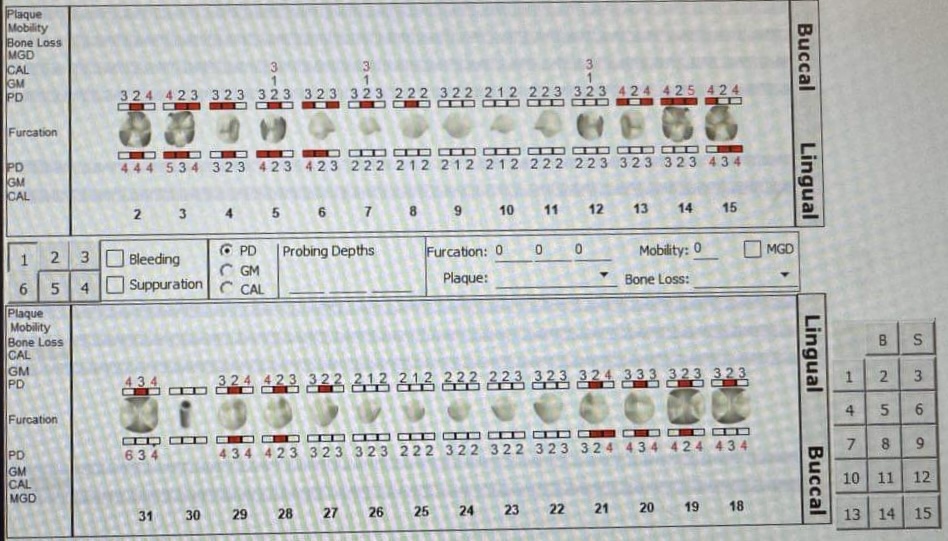
Periodontal assessment: Gingival margin is at the CEJ and localized gingival recession 1-2 mm, generalized red color gingival papillae, rolled in shape, shiny and non-stippled in texture, non-resilient in consistency. Generalized inflammation is the gingival margin.
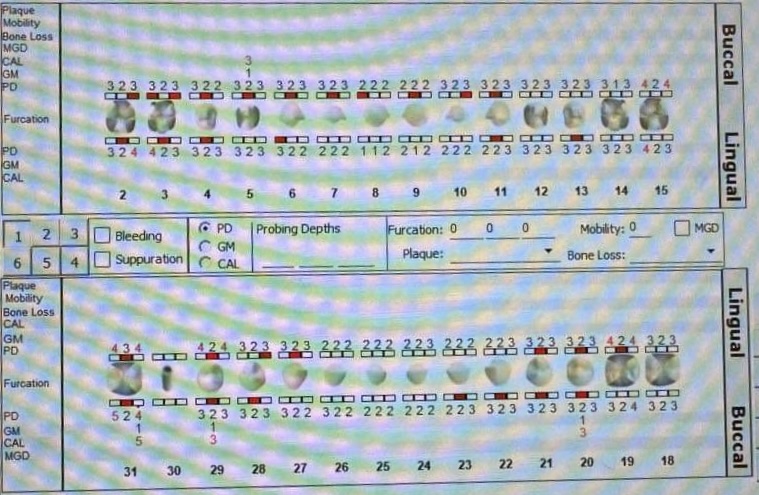
Perio charting: Localized 2-4 mm pocket depths and localized 5-6 mm pocket depths teeth #3-D, 14-D and #31-D. Localized 1-2 mm gingival recession. Generalized bleeding on probing. Calculus: Moderate supragingival calculus localized on teeth #22-27 lingually and generalized heavy subgingival calculus. Light extrinsic stains yellow color on posterior teeth.
Before treatment.
After treatment.
The patient’s periodontal status was diagnosed as Periodontitis, Stage 1, Grade B. Heavy case value.
Based on all assessments the treatment and homecare plan were developed and discussed with the patient. The patient was given oral hygiene instructions, recommending the use of a power toothbrush twice a day by Modifed Bass methods for 2 minutes using fluoride toothpaste, daily using interdental flossing, rinsing the mouth twice a day with mouthwash Listerine, and daily tongue cleaning. Treatment with Arestin on-site was approved for a 5 mm pocket depth after scaling all quadrants.
Implementation
Hand and ultrasonic scaling were performed in 1 and 4 quadrants in one visit and 2 and 3 quadrants in the next visit for pain management using topical anesthetic gel 5% Lidocaine. Arestin was then administered at the site of tooth # 14-D. The patient received Arestin post-treatment instructions on November 4, 2023.
Evaluation
The re-evaluation of tooth # 14-D (3mm) after treatment with Arestin identified a reduction of pocket depth from 5 mm to 3 mm on February 3, 2024. Hand and ultrasonic scaling were performed, followed by coronal polishing and application of 5% fluoride varnish. Treatment with Arestin was recommended to the patient to achieve the main goals of reducing pocket depths and inflammation, with the overarching aim of maintaining and stabilizing oral health and preventing the progression of periodontal disease. After comprehensive periodontal therapy such as treatment with Arestin, improvements in daily oral home care practices and regular professional scaling procedures every 3 months are necessary to achieve optimal outcomes in periodontal health.

Before treatment.

After treatment.


