74 year old African American female presented to our Dental Hygiene clinic for her recall visit.
Medical History:
Upon reviewing her medical history, the patient stated she is taking 4 different medications for high cholesterol, anxiety, and high blood pressure. These medications included Atorvastatin 20mg-1x/day, Lisinopril 40mg-1x/day, Buspirone 10mg-3x/day, and Amlodipine 5mg-1x/day. Due to the patients anxiety, I decided to go over her social and dental history before checking vitals and offered her some water. The patient stated she was a non-drinker and non-smoker who received her last cleaning 3 months prior to her current visit, in November of 2023. The patient stated her home care routine consisted of brushing 2x/day with an electric toothbrush, Paradontax toothpaste and flossing about 5x/week with a floss pick. The patients vitals after that time was: 134/74 P: 60, corresponding to Stage 1 Hypertension. The patient stated she had not yet taken her blood pressure medication until she arrived that morning.
The patient was classified as an ASA 2, due to her blood pressure, cholesterol and anxiety.
Assessment/Oral Findings:
EO/IO: A comprehensive dental exam was done, including an extraoral and intraoral examination. Bilateral clicking of the jaw was noted, being asymptomatic. During the intraoral exam, a red lesion on the mesiofacial surface above #8, about 3mmx5mm in size was detected. The patient stated she had a biopsy done in 2022 and everything came back normal. Bilateral mandibular tori, bilateral trauma of the buccal mucosa, a fixed mandibular retainer and a white raised nodule about 1x1mm in size on the labial mucosa was noted; all asymptomatic.
Dental charting: The patients class of occlusion was determined to be class 1 on the right side and class 2 on the left size, with an overjet of 2mm and overbite of 10%.
Gingival assessment: Gingiva appeared pale pink with hyperpigmentation, generalized rolled papillae with a soft consistency and smooth texture.
Calculus detection: Light deposits of subgingival calculus were detected with mild brown and yellow staining present on the anterior lingual surfaces.
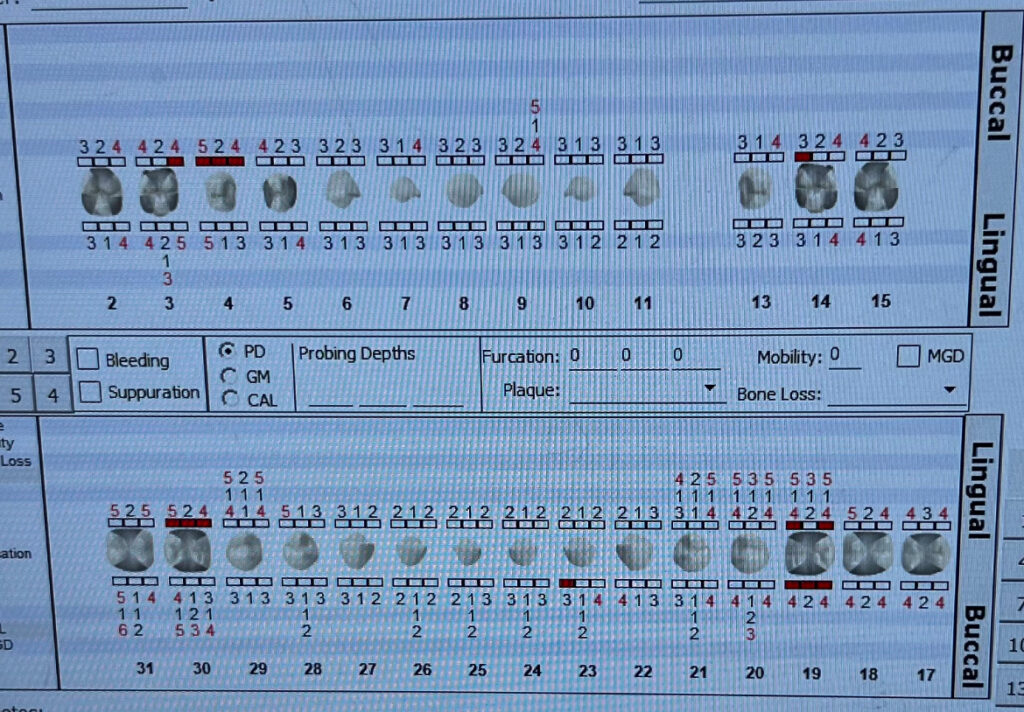
Periodontal charting: During the last recall visit in 2023, the patient was given a comprehensive dental exam and upon perio charting it was determined the patient qualified for Arestin. The Arestin was administered in 4 posterior sites with 5mm readings; #19-DB, #19-DL, #29-ML, and #30-DL. The patient had generalized 3-4mm PD with localized 4-5mm PD, and 1-2mm of gingival recession present.
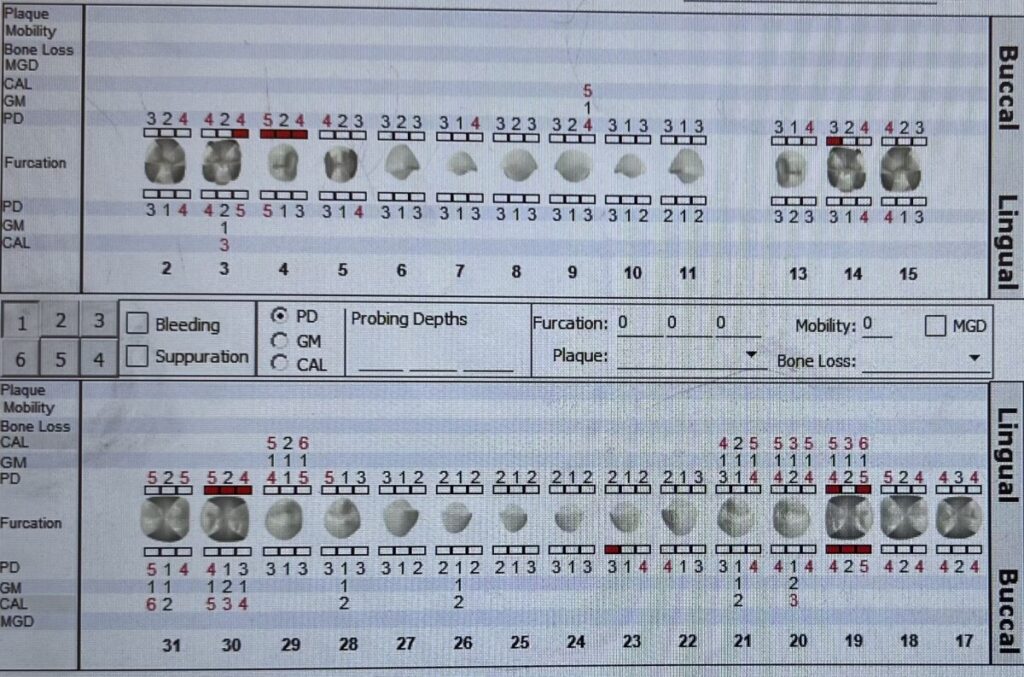
A new perio chart was created to re-evaluate the patients probing depths, as well as the sites where Arestin was administered. Additional areas of localized recession was noted as well as a 1mm reduction in 3 of the 4 Arestin sites. 4mm readings were noted on #19-DB, #19-DL, and #29-ML. #30-DL remained with a 5mm PD. The patient stated that this change encouraged her to commit to her home care and regular recall visits.
Due the last series of radiographs being taken 2 years ago at another facility and no current radiographs present at our clinic, a set of 4 horizontal bitewings were taken.

Radiographic findings: No radiographic calculus or caries were noted. Generalized horizontal radiographic bone loss of about 30% was noted. All findings were discussed with the patient.
After all assessments were completed, the patients case value, perio status and caries risk were determined. The patient was a Light, Stage 2 Grade B Periodontitis case with a high caries risk due to existing restorations and experiencing xerostomia due to medication. A treatment plan was developed and discussed with the patient to go over oral hygiene care and well as scale the mouth to completion in one visit. It was essential that we took the time to go over the importance of oral home care, including the continuation of brushing 2x/day with a Fluoride based toothpaste, incorporating the proper flossing technique and type of floss for plaque removal interproximally as well as for the fixed retainer, and the use of a fluoridated mouth rinse. The patients questions were answered and it was imperative that the patient demonstrated proper use and understanding prior to moving on.
In the continuation of treatment, the patients teeth were polished after scaling. The patient initially declined the application of Fluoride varnish due to an article she saw online, however asked for my professional opinion. After taking some time to explain the purpose, function and benefits of the Fluoride Varnish, the patient decided she was comfortable receiving the treatment.
This case demonstrated the importance of empathy, compassion, and dedication within each case. No matter how complex or simple the case, keeping the patient involved in their own case and educating them as well as making the feel comfortable is far more valuable. This was important during this case to reduce the patients anxiety and ensure their full autonomy as opposed to experiencing fear. Every case is individualized and to know your patient and their needs can help you determine the best course of care.



