70 year old African American female presented to our Dental Hygiene clinic for her cleaning with a chief complaint of pain and swelling in the maxillary anteriors.
Medical History:
The patient stated she is taking medication for type 2 Diabetes, high blood pressure, and nerve pain. These medications include Trulicity 1.5mg/0.5mL pen injector 1x/week, Metformin 500mg-2x/day, Carvedilol 25mg-2x/day, Hydrochlorothiazide 25mg-1x/day and Lyrica 100mg-2x/day. The patient was given some time at the beginning of the appointment to relax and drink some water prior to vitals being taken and reported she ate prior to coming in. The patient stated she reports no side effects from the medication, no recent hypo/hyperglycemic episodes, and her last HbA1C reading was 6.3% a month ago. The patient stated she was a non-drinker/non-smoker whose last cleaning, radiographs and dental visit was 4 years prior. The patients reported home care consisted of brushing 1x/day, using a water flosser instead of floss 1x/day and Listerine Antiseptic mouth rinse 1x/day. The patients vitals read as 168/95 P: 75, corresponding with Stage 2 Hypertension. The reading was re-assessed 5 minutes later: 144/88 P: 70. The patient reported she takes her medication at night and did not take it that morning. It was determined the patient would only receive non-invasive assessments due and continuation of treatment would begin the following appointment.
The patient was classified as an ASA 2 due to high blood pressure, diabetes and the medications taken for it.
Assessments/Oral findings:
EO/IO: After completing the extra-oral exam, a mobile lymph node was noted as present in the patients neck as asymptomatic. The patient presented with a scar on the left side of her neck due to a tracheostomy from 2003. Right side clicking of the jaw with deviation to the right upon opening was also noted; asymptomatic. The intro-oral exam revealed bilateral mandibular tori, linea alba preset on the right side and scalloped borders of the tongue present.
Dental charting: The patients class of occlusion was determined to be class 1 on the right side and class 2 on the left side, with an end to end underbite and cross bite. Moderate attrition localized to the mandibular anteriors were noted, as well as multiple fractures of posterior teeth.
Gingival description: The patients gingival assessment demonstrated generalized severe inflammation, most prominent along the gingival margin of #6-#10 where a bridge was present. Red gingival tissue with generalized bulbous papillae, and a smooth, spongy consistency was also noted.
Calculus detection: Generalized moderate deposits of subgingival calculus were detected with moderate supragingival calculus localized to the mandibular anterior linguals.
Periodontal charting: Moderate bleeding upon probing was present with generalized 2-4mm PD and 5mm PD localized to the posterior regions.
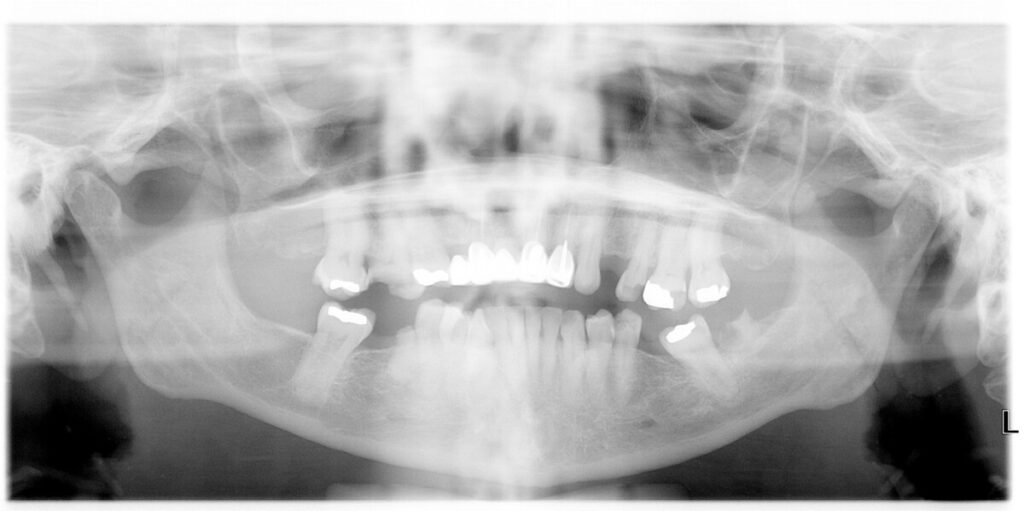
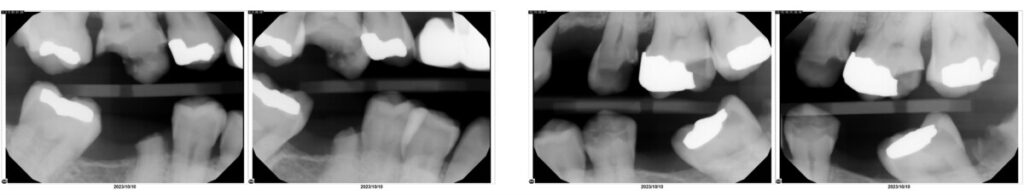
Radiographic findings: Radiographic calculus present in localized areas. Localized horizontal radiographic bone loss between 15%—33% present. Retained root tips noted on #17 and #30. Multiple areas of decay noted. No periapical pathology or jawbone abnormalities were noted. Patient was informed and aware of findings.
After all assessments were completed, the patients case value was determined to be a medium with a high caries risk. The treatment plan was developed and it was planned to expose a PAN and 4 horizontal bitewings on the 2nd visit, as well as begin debridement of quadrants 1 and 4. The third and final visit was planned to re-evaluate tissue and scale quadrants 2 and 3 to completion. Pain management was implemented using Oraqix (2.5% Lidocaine, 2.5% Prilocaine) as the patient declined local anesthesia. The patient responded well during the debridement of areas that displayed inflammation, excessive bleeding and exudate. Each appointment was scheduled for an afternoon/evening visit to reduce the stress and allow the patient time to eat, take her medication and avoid rushing.
With each appointment, plaque index and oral hygiene instructions were emphasized; including brushing 2x/day with the proper brushing technique, flossing with the proper method as well as the introduction and demonstration of super floss to educate the patient on how to clean beneath her bridge. The patient was informed of the link between oral health and systemic health, as well as the risks increased with having diabetes. An adult referral was given for carious lesions, restorative care, and stage 2 hypertension. The patient received a 5% sodium fluoride varnish treatment and was scheduled for a 3 month recall revisit.
This case demonstrated the importance of critical thinking and the knowledge on health conditions that may be present in future patients. This allows me to know the right questions to ask for a detailed medical history, as well as how to go about this specific case in a manner that benefits the patient while making them feel as comfortable as possible. It is common for a patient to feel insecure or unaware of their current oral health state. Showing compassion, empathy and patience while also educating them allows the patient to feel safe and informed.



