An Oral Pyogenic Granuloma is a benign, inflammatory lesion involving rapid growing gingival mass that has the potential to react to a variety of stimuli. The lesion appears as an isolated, discrete, soft, round enlargement near the gingival margin usually associated with the interdental area. It tends to form a mushroom-like shape, with a smooth glistening surface. Typically, the color of the lesion depends on the age of the lesion, with newer lesions having increased vascularity. This lesion bleeds readily with slight trauma but is often painless until it interferes with mastication and or occlusion. (Wilkins’ 13th Edition Clinical Practice of the Dental Hygienist)
My clinical experience:
PATIENT PROFILE: Mr. R is a 43-year-old Caucasian Male. He lives in Brooklyn NY. He came to the dental school clinic for a routine dental cleaning.
CHIEF COMPLAINT: “I need a cleaning”.
PAST DENTAL HISTORY: The patient was last seen by a private dentist in 2019 for a restorative crown procedure. Last dental radiographs were taken in 2019 during the crown procedure. Last dental cleaning was performed in the later months of 2019. Pt. reports dry mouth at night and generalized sensitivity to hot, sweet, cold, pressure. Pt. reports slight pain in the lower left where the new crown was placed as well as pain on the upper left in the back (#15).
MEDICAL HISTORY SUMMARY: ASA II. Mr. R reports taking Adderall (5mg) for ADD and Zoloft/Sertraline (100mg) for depression and no OTC meds/vitamins. Mr. R reports no allergies and last physical exam was in 2021 with good health overall. Mr. R reports non-drinking and smokes marijuana daily.
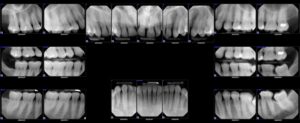
CLINICAL FINDINGS: Extra-oral examination: Mr. R presented with a small 1mm scabbed herpetic blister on the left lip commissure. Pt. stated that it was asymptomatic. Pt. stated that a benign mole was removed fro his left occipital region in 2021. Intra-oral examination: Observed on Mr. R was a diastema between #8 & 9, bilateral hyperkeratinized retromolar pads on the mandibular arch, and mild bilateral mandibular tori. Also observed during Mr. R’s intraoral examination was a localized enlarged interdental gingival lesion between #22 & #23. Pt. stated that he has been aware of enlargement since 2012 and states that it has tripled in size since first noticing it. Oral pathologist Dr. Gwen Cohen-Brown was available for consult and determined it was a pyogenic granuloma. An image was taken for documentation purpose. Dr. Brown advised Mr. R to monitor the lesion but it may need surgical removal in the future. Gingival assessment: Mr. R had generalized pink stippled gingiva, with mild marginal gingival inflammation. Gingival margins appeared rolled on lingual surfaces. Papillae is slightly inflamed. Periodontal findings: Pocket depths were measured generalized 1-3 mm with localized 4-5 mm pockets observed on the posterior molars/premolars. Minimal BOP. Minimal mild calculus detected. Mild supragingival calculus detected on the lingual and interproximal surfaces of the lower anteriors. Mr. R’s PI score was 0.7 (fair) with marginal gingival biofilm accumulation. Radiographic Findings: Incipient caries observed interproximal on #30D, #31M, calculus observed on M&D surfaces of lower anterior dentition. No radiographic bone loss observed. Possible open margin on D of #19 crown. No PAP or jaw bone abnormalities noted.
PLANNING: 2 appointments were scheduled to complete Mr. R’s dental cleaning. Appointment 1 consisted of completion of all patient assessments, FMS exposed, OHI recommendation for GUM soft interdental picks especially for interproximal areas where food accumulation occurs- Mr. R demonstrated proper technique. Hand scaled along with use of ultrasonics for cleaning completion in Q1. Appointment #2 consisted of review of OHI and introduced c-shaped flossing method where Mr. R demonstrated proper technique. Cleaning in remaining quadrants was completed using hand instruments and ultrasonics. Engine polished all 4 quads with med. grit prophy paste and 5% sodium fluoride varnish was administered to both maxillary and mandibular arches- post op instructions were given to Mr. R. An Adult referral was given to Mr. R for suspicious lesions on #30D & #31M.
IMPLEMENTATION: The treatment proceeded as planned and the patient was receptive to documentation procedures. No skill roadblocks were encountered with dental health education. The patient was able to demonstrate adequate skills using the GUM soft interdental pick and string floss. Mr. R’s PI score decreased slightly at his 2nd appointment. Hygiene procedures were accomplished with a minimum of difficulty. Photographs were taken and permission was obtained to use them.