Patient X is a 35 year old male who presented to the clinic as a heavy cannabis smoker. The following breakdown of the case includes gingival descriptions, treatment plan, improvements, intraoral photos and continued care recommendations.
CC: “No current complaints, just here for a cleaning”
Health History Overview:
-
-
- Vitals: BP reading is within normal limits. 120/78, P: 83.
- Medical conditions: No current conditions
- Medications: No current medications
- Social history: Pt smokes cannabis daily (2x/day) but no other tobacco, drugs or alcohol use.
- Dental history: Pt reports using a manual toothbrush 2x/day, doesn’t floss but occasionally uses mouthwash (Listerine). Pt didn’t report any current complaints regarding his oral hygiene, just very minor, sporadic sensitivity to extremely cold foods. Pt reports he last received a dental exam, and cleaning, including dental images approximately 5 years prior to the visit.
-
EO/IO:
EO: Slight. 3 mm moveable, painless and palpable suspicious swelling in his right clavicular region and similar, painless, moveable submandibular swelling. Evaluation done by supervising dentist. Pt palpated area and was advised to consult with PCP if not resolved after two weeks.
I0: Mild tori on hard palate.
Dental Charting:
Gingival description:
Gingiva appeared hyperkeratotic, with localized bulbous gingival tissue on mand/max incisors with localized cratered papilla near mand/max premolars. Gingiva is puffy, friable, and appears fibrotic with bleeding and exudate present upon mild palpation. GM appears coronal to the CEJ. Generalized severe inflammation.
Periodontal charting:
In considering that the pt hasn’t had radiographs exposed in 5 years, exudate present near the max. anteriors BW’s and 4 PA’s were exposed.
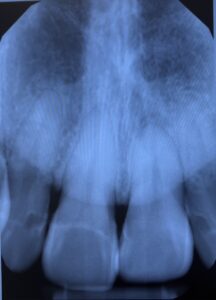
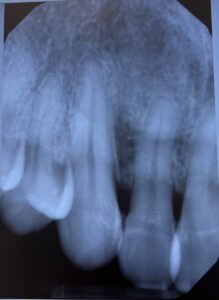
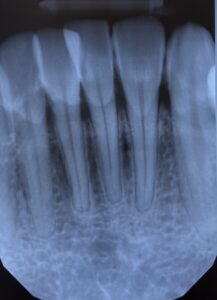
Radiographs:
Intraoral images:
Images taken during initial visit.


Dental Hygiene diagnosis:
Periodontal status: Stage II Grade C
Caries risk: Moderate
Dental Hygiene Care Plan: The patient was during my first semester seeing patients so multiple revisits were required. Six total visits were done, with polishing and 5% fluoride varnish applied on the last session. Pt refused local anesthesia. Each sextant was scaled per visit, with rescaling done on each visit due to decrease of inflammation and presence of residual calculus.
Implementation:
Visit #1: Reviewed medical, social, dental history. Completed dental, period charting. Exposed 4VBW’s.
Revisit #2: Completed PI, OHI, scaled to completion teeth #6-11. Exposed PAs. Referral for apical radiolucency and bone resorption was provided.
Revisit #3: Evaluated for residual calculus in sextant 2. Scaled QI to completion, began scaling QII. Heavy calculus removed from #25, 26 facial.
Revisit #4: Assessed gingival tissue, evaluated for residual calculus. PI. Discussed modified Bass method, smoking cessation & proper WaterPik usage. Scaled to completion QI, QIV and mandibular anteriors.
Revisit #5: Evaluated gingival tissue, and residual calculus. Completed full mouth scaling. Discussed OHI & smoking cessation.
Challenges during treatment:
With no local anesthesia to control bleeding, treatment needed to be done slowly to ensure that blood and exudate was being monitored and continuously cleaned.
Patient also continuously smoked during treatment which caused the presence of more staining during the treatment process.
Final reflection:
The biggest challenge during the treatment process was the patient’s smoking habit. However, through conversations targeting smoking cessation the patient was able to decrease smoking from 2x/day to 1x/day. After his visits at NYCCT Dental Hygiene clinic the patient made the transition from manual tb to an electric tb, began incorporating a water flosser into his routine and committed to changing his smoking habits.
 Third molars were erupted and visual clinically. Pt didn’t have any crowns, or implants. Suspicious carious lesions were detected on #1-O, #2-O, #14-M, #30-O, #32-O.
Third molars were erupted and visual clinically. Pt didn’t have any crowns, or implants. Suspicious carious lesions were detected on #1-O, #2-O, #14-M, #30-O, #32-O. 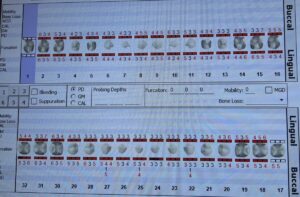 Generealized BOP and exudate. Localized 5-8 mm PD in posterior teeth, and localized 3-4 mm PD in anterior teeth.
Generealized BOP and exudate. Localized 5-8 mm PD in posterior teeth, and localized 3-4 mm PD in anterior teeth.  Radiographs revealed there was no active infection. Apical radiolucency and bone resorption on #9 was observed. Apical resorption present #24,25,26 with suspected trauma. Pt states he used to be a boxer. Generalized interproximal calculus, generalized 15-33% horizontal bone loss with localized vertical bone loss between #1,2,3-M.
Radiographs revealed there was no active infection. Apical radiolucency and bone resorption on #9 was observed. Apical resorption present #24,25,26 with suspected trauma. Pt states he used to be a boxer. Generalized interproximal calculus, generalized 15-33% horizontal bone loss with localized vertical bone loss between #1,2,3-M.