My name is Florentina Lubani and I was born and raised in Montenegro, a small country in Eastern Europe. I came to the United States five years ago, when I was 18 years old, with my family, my mom, dad and my three sisters. Coming from a country not well developed financially to a country that offers people many possibilities, got me stuck to the idea that I would never make my dream come true. The dream of becoming a dentist! The reality of having “4-time braces” in my life, made me love this profession more and more because I got to know it better.
But what about my English? Oh God, I always said two words would not make me an English speaker. Yes, I knew and understood only “Hi!” and “Bye” and don’t feel shy about that because these words gave me willpower to learn more. Day by day I felt very unprepared financially to start dentistry. Leading a family of four daughters younger than me was not easy when you start a whole new life in a big different country. I felt very bad for my father and mother to make them pay for my expenses, so I checked on the internet about a profession related to dentistry with fewer expenses and I found this Dental Hygiene program. I never heard about this profession before because is not classified as a major separately in Europe, so I searched about it more in details. I liked the explanation of hygienists as primary healthcare professionals who work alongside dental professionals to provide treatment of oral health care. With my heart full of happiness, I said yes this is it.
In Fall 2015, I got registered at ALCC American Language for ten weeks to learn and improve the language, and in Spring 2016, I registered at CUNY Language Immersion Program known as CLIP at City Tech to take my ACT test and register for college classes. I was lucky and passed reading, writing and Math classes and applied for dental hygiene pre-requisites for fall 2016. I completed all my pre-requisites in City Tech, and in June 2018 I received the letter of my acceptance in dental hygiene. I cried from the happiness because I’ve been waiting for the letter for days.
With the start of the program, I started to work in one dental office in Ridgewood Queens as a dental assistant. Every afternoon after classes going to work, felt very good and could not wait to go. The dentist was very helpful and motivated me to do better in my major.
About two years in this program, from August 2018 until March 2020, every day was a wonderful learning experience from the staff of the program and my dear patients. Being able to provide all my knowledge in the clinic three times a week, made my skills stronger in clinical practice, communication and professionalism. Clinic helped me to improve my ergonomics and instrumentation techniques every time that I had to treat my patients. A favorite part of clinic was educating patients about proper toothbrushing, flossing and rinsing techniques, and how important these methods are for daily life. This program has strengthened my critical thinking and desire to become a strong future dental hygienist.
My first patient was my third sister, Florjeta. Even though my skills were not strong during that time, I was very excited to bring her in the clinic and show her my cubicle and what I do. I felt like a kid who wants to show her toys to a member of the family.
What would I do without her? Her name is Winsome, one of the most perfect humans in the world. When I think about her, I say: “It’s not what we have in life, but who we have that matters!”. I met her in August 2016 on the program’s orientation day. Since that day she became a special friend, a person who makes me laugh, protects me, supports me, makes me believe that there are good things in the world, that there is an unlocked door waiting for us to open it, and her hand was there to hold mine and got me through my hard and confused times. We got to hang out a lot, and I made her eat my favorite Balkans food “Burek”. Winsome got to be part of my wedding as well and she dance an Albanian “shote” with me.
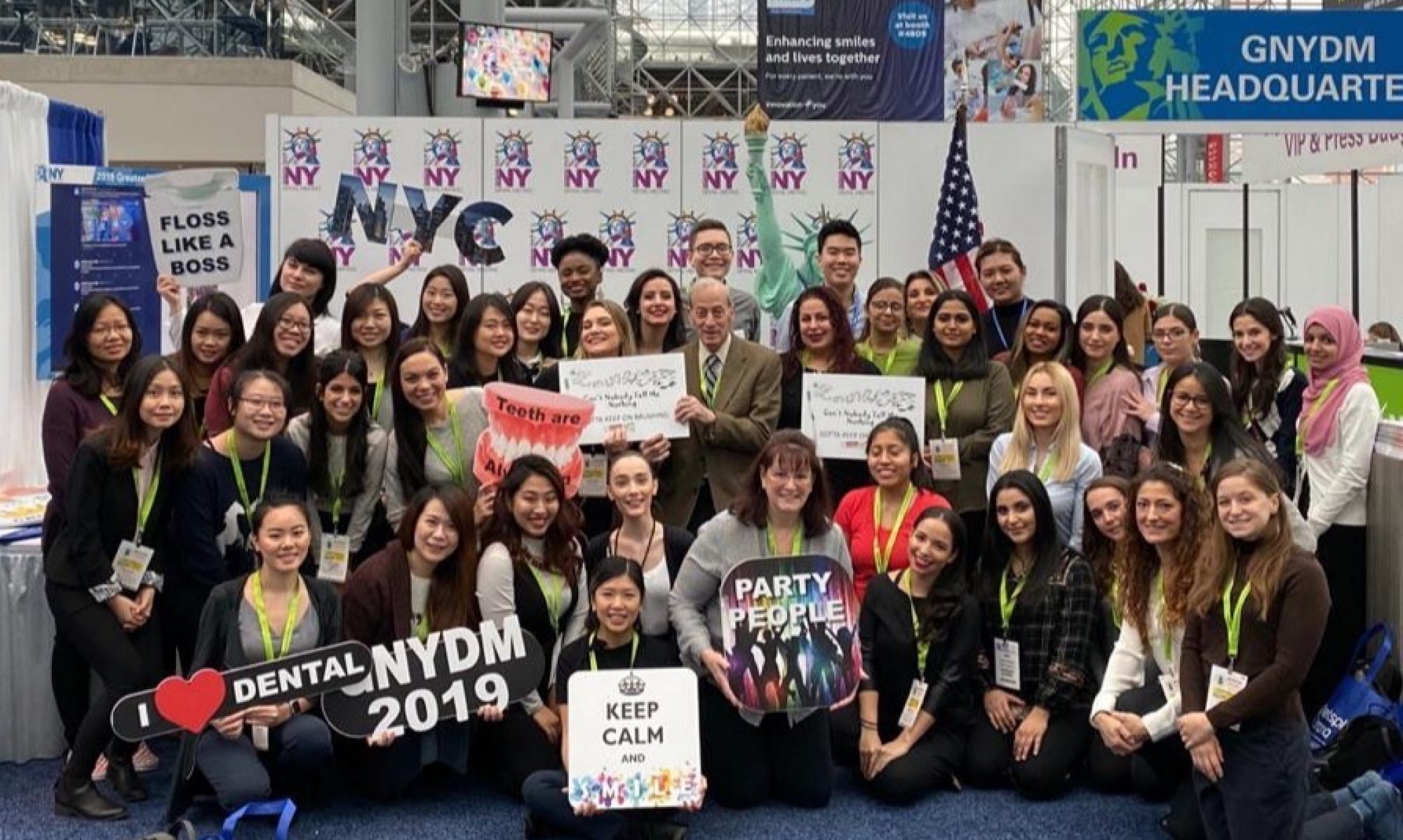
Also, in the first semester, students of dental hygiene program were invited to participate in Greater New York Dental Meeting 2018 (GNYDM), in the largest Dental Congress in the world at the Jacob K. Javits Convention Center. I was so excited to be part of that tour cause I got to learn and see interested things about dentistry. I volunteered with some of my classmates to model for “Twice as Nice Uniforms” organized by Crest and OralB. We modeled about their brand-new uniforms in front of the people who were interested about their products. We had so much fun!
In my second semester of Dental Hygiene program for seminar class, me and my two other classmates were chosen to do a research study about Periodontal Disease and Down Syndrome. First, we did the presentation in front of our classmates and then on another day we did it in the cafeteria of our campus. During the presentation, students and faculties from the college approached us by asking many questions about the periodontal disease that they never heard before and how it affects people with Down Syndrome.
The experiences that I had in this program are numerous, and I am glad that I had to live all of them. I was chosen as a day class representative by students for SADHA. SADHA is an abbreviation for Student American Dental Hygienists’ Association where students connect with their future professional organization. Our SADHA group planned a goodbye ceremony for our senior students and that day was an unforgettable day.
In the beginning of third semester, on August 19, 2019, I volunteered to participate for “New Student Welcome”, headed by Dr. Lorna Flamer-Caldera, as a student leader. I had to explain the importance of how to get the NYCCT information through CUNYfirst, Open Lab, Blackboard, and creating and checking CityTech email daily. Also, an important discussion was on how to focus on academic success at CityTech, while going to class, doing homework, being organized, knowing the requirements of classes and due dates, and the purpose of a “faculty office hours”. A lot of different questions about dental hygiene program were asked by the new students who were interested about the program, and I felt wonderful on answering their questions.
Throughout all the amazing experiences that I had, it’s worth mentioning SADHA toothbrushing sale where a lot of students from City Tech bought our products. Not only SADHA participant participated in that day, but also other seniors from our dental hygiene program helped us to sell many toothbrushes, flosses and mouth rinses. In the end, we all were very happy on the amount of the products that were sold.
I was chosen by the chair of the department to be a demonstrative patient for Colgate tooth whitening system, where the Colgate Corporate representative came to teach the DH faculty about this new product for whitening and provide patient demonstration. This system taught and prepared me as well for the clinic in the Spring semester.
Two procedures that I loved to do in the clinic were removing sub and supra gingival calculus and placing sealants. The reason why is because with removing the calculus I can save patients from getting gingivitis and periodontal disease, and with getting sealants patients would avoid tooth decay and keeping out germs and food.
A research that I have done in the third semester in Oral Pathology, was about Minor Apthous Ulcer. Minor aphthous ulcers, which is also known as Mikulicz ulcers, are the most common type of aphthous ulcers. Primarily, they appear in childhood and/or adolescence, and are less than 1 cm. Minor aphthous ulcers can form as a single ulcer or in a cluster, but its exact cause remains unclear. Many researchers suspect that a combination of factors contributes to the sudden appearance of minor aphthous ulcers. This includes: minor injury to the mouth from dental work, brushing, accidental cheek bite, toothpastes and mouth rinses that contains sodium lauryl sulfate, acidic foods, a diet lacking in vitamin B12 or iron, an allergic response to certain bacteria in the mouth, hormonal shifts during menstruation and emotional stress. Minor aphthous ulcers may also occur due to certain conditions and diseases such as Celiac disease (intestinal disorder), Crohn’s disease (inflammatory bowel disease), Behcet’s disease (a rare disorder that causes inflammation throughout the body), a faulty immune system that attacks healthy cells in the mouth (viruses and bacteria) and HIV/Aids which suppresses the immune system. “Clinically, it presents as extremely painful, shallow ulcerations with an erythematous halo on unattached oral mucosa.”1 They begin as pale yellow in color and, as the condition develops, they turn grey. May also be ringed with red or fully red when inflamed. In one oral diagnosis service study of the Rio Grande do Norte Federal University in Natal age, sex, race and laboratory test results were collected. Of the 68 cases with aphthous ulcers, 40 were females and 28 males with a mean age of 41.9 years. The mixed-race people were the most frequent (30), followed by Caucasians (23) and African-American’s (9), being this information unavailable in 6 cases. A biopsy is not necessary unless there is a lack of improvement of the minor aphthous ulcers within two weeks. A swab is essential to exclude viral, bacterial or candida (thrush) infection. There is no laboratory exam for minor aphthous ulcers diagnosis, but full blood count, dosage of inflammatory and hematological markers and vitamins and serologies are useful tools to rule out systemic conditions that can cause it. In general, minor aphthous ulcers are non-serious conditions which will go away without any treatment in a couple of weeks. But the main goal of treatment is to ensure adequate nutrition and prevent ulcers from recurring. Protective pastes, antibacterial mouthwashes, avoiding toothpaste with sodium lauryl sulphate, reducing stress, ensuring soft or liquid diet and correcting vitamin deficiencies may also help on treating minor aphthous ulcers. If they heal on their own within a few weeks, they are not an indication of oral cancer and are non-infectious. But, if the minor aphthous ulcers does not heal within two weeks, or last longer than two weeks, the affected person should see a doctor for diagnostic workup because in some cases, a persistent ulcer may indicate oral cancer. “Chronic oral ulcers may be drug-induced, or due to benign or malignant tumors. Every oral solitary chronic ulcer should be biopsied to rule out squamous cell carcinoma. A solitary palatal ulcer can be related with necrotizing sialometaplasia.”2 Applying a strong topical corticosteroid frequently throughout the day or topical analgesics, can help with pain relief and wound healing. “Alternative topical options include tacrolimus or tetracycline or superficial cauterization with silver nitrate. In severe cases, oral prednisolone may be given. Other medications that have been effective in controlling symptoms, include oral tetracyclines, colchicine, pentoxifylline, dapsone, azathioprine, methotrexate, cyclosporin and thalidomide. Biologic agents such as adalimumab, etanercept and infliximab have also been reported to help in severe resistant cases.”3 The diagnosis of minor aphthous ulcers is difficult due to its similarities with mucocutaneous lesions. Differential diagnosis with herpes, chickenpox, erythema multiforme, erosive lichen planus with ulceration, pemphigus vulgaris and pemphigoid is based on the clinical appearance, location and course of the ulcerations. Minor aphthous ulcers are also confused with traumatic ulcers. It is related to us as dental hygienists because it mostly occurs in oral mucosa.
Participating in the New York Smiles 2019 program at the GNYDM, was one of the most fun-loving experience. I was chosen to sing with few other dental hygiene senior students about children from elementary school who came specially with their teachers for oral hygiene education and dental screening. They were very happy to sing and dance with us the phrase: “Can’t nobody tell me nothing, gotta keep on brushing!” and we were happier to bring happiness on their face.
An experience I have had in clinic was a 72 year-old Caucasian male patient who stated that he uses soft manual toothbrush twice a day with Colgate Total toothpaste and flosses rarely. This patient was a pipe – smoker for 45 years and smokes 15-20x/day. I took his vitals and his blood pressure was 100/79 and his pulse was 67. In 2007 he had radiation therapy for prostate cancer and in 2015 was diagnosed with hypothyroidism. Other medical conditions were vasovagal syncope, triglycerides and was allergic to Penicillin. My patient’s current medications were: Levothyroxine 0.025mg bid for thyroid deficiency, multivitamin, Polyvinyl alcohol 15ml qid for dry eye(s) and Fish oil 1.000mg bid for triglycerides. Extraoral examination was within normal limit and in intraoral examination slightly red palatal tonsils were observed, bilateral linea alba, slightly coated fissured tongue, short lingual frenum and a scar on the left side of hard palate was evident. He has had localized mild attrition from #22 to #27, bilateral class I of occlusion, overbite 60% and overjet 4mm. Also, my patient has had generalized moderate brown stains and localized mild black stains, and generalized plaque around gingival margin and localized supragingival calculus. Generalized red inflamed rolled and bulbous gingiva were observed with 2-5mm probing depth and generalized moderate bleeding upon probing. He was periodontal type II active due to the localized recession on the fifth sextant. My patient was at high risk of developing stains again if he does not start reducing and/or quit pipe-smoking. The main issue with which he can be faced, is the risk of developing chronic obstructive pulmonary disease. Related to this, he also stated that many times he gets short breath, when for example, he tries to catch a bus. He came for dental treatment twice. On the first visit, after finishing the assessments, I started teaching him oral self-care instruction. I chose teaching the Bass method toothbrushing technique to remove dental biofilm adjacent to and beneath gingival margin. Ater OHI, I started scaling with ultrasonic device, quadrants III and IV. I kept my patient in semi-supine position while working in the quadrants mentioned before and everything was going normal. Around 3p.m, while I was removing the supragingival calculus and the stains on the lingual of sextant 5, he started to cough, his face became purple, with eyes and lips slumped over, and did not respond for 30 seconds. I did not leave from my cubicle, but I called my professor who was helping another student to come over. Within seconds he responded back like nothing happened and was willing to continue treatment. We terminated treatment and sat the patient up. The doctor on that clinic day did a quick intraoral inspection to determine if any crowns were swollen, but there was no dental work missing. My faculty and I proceeded to take his vitals two more times and each time it was elevated (on the second time 130/96 and on the third time 140/108). We also offered to send the patient home with an Uber because he lives alone, but he refused. We referred my patient to his primary care physician to have a neurological and cardiology work up, and he needed a note from his physician to return for dental treatment. My patient came to the clinic to make an appointment for his second visit and brought his medical clearance. In his medical clearance, it was written that the patient was suffering from vasovagal syncope, which is a benign condition, and he can continue to receive dental care as before but had to avoid head-down position. Due to unfinished procedure on the last visit, there was generalized residual plaque and stains and localized interproximal calculus. To him I recommended re–care in 3 months because he did not have an intention to stop pipe-smoking and the stain will continue to develop again. I did discuss with the patient the reasons why he should quit pipe-smoking and all the negative effects that it can cause primarily in the oral cavity, but he responded to me saying “I am 72 year old and still alive!”. What went right in the second visit is that I worked standing up while I used ultrasonic and the patient position all the time was I semi-supine. After cleaning every two teeth, I kept asking if he felt fine during the treatment. Also, what went wrong is that in the first visit my patient did not gave us all the information for his medical and social history, and he did not tell me that he feels uncomfortable in the position that he was. What I could do differently is working on him every time standing up and not like in the first visit siting on the chair and paying more attention in the suction while most of the time does not work.
My experience with Pedo patient was wonderful. A 4-year-old little girl brought joy and happiness with herself while she was sitting in the chair. All her primary teeth were erupted and were pure white, as she said: “My teeth are white like rice”. No early childhood caries was detected, and she was happy that she did not have any germs on her mouth. It was her first time to a dental clinic, and I was very surprised how she was not shy. Of course, I had to familiarize her with the environment first, but she liked it.
Placing Arestin, which is an antibiotic added on to scaling and root planning procedures to reduce periodontal pocket depth, was a requirement on the third semester, but I was not lucky to have a patient qualified for it then. I was able to place this antibiotic on the fourth semester to one of my classmate’s patient on February 13, 2020 approved by Dr. Brown, the faculty on that day in the clinic. Unfortunately, I was not able to evaluate the placement of this antibiotic due to the college closure from Covid-19.
There was not everything light. There were days that we felt exhausted and did not want to be in the campus. There were clinical days that our patients did not show up and we cried from the anger, but also days that we said: “That’s fine, I got used with this!”. But as students, we loved each other, we supported each other, we became a family together, and we spent most of the time there, together. I will miss everyone terribly!
In the end I go back and think, how many hours, days, weeks, months and even years for us to get the title of RDH? Life in this program taught me that it is not about how fast I get there, but how I taught myself not to give up and trust in the process of making my dreams true. In the day that I brought my dad in the clinic to be my patient, he told me: “Tina, thank you for making me proud!”. This was my favorite quote since that day. After every hardship, there is a light in the end of the tunnel.
I made it. We made it. Horray !