Contents
- 1 History of Mental Illness
- 2 History of Mental Illness
- 3 Diagnosis of Mental Illness
- 4 Therapeutic Orientations
- 5 Introduction
- 6 Psychoanalysis and Psychodynamic Therapy
- 7 Humanistic and Person-Centered Therapy
- 8 Cognitive Behavioral Therapy
- 9 Acceptance and Mindfulness-Based Approaches
- 10 Emerging Treatment Strategies
- 11 Pharmacological Treatments
- 12 Integrative and Eclectic Psychotherapy
- 13 Conclusion
History of Mental Illness
Hood College
This module is divided into three parts. The first is a brief introduction to various criteria we use to define or distinguish between normality and abnormality. The second, largest part is a history of mental illness from the Stone Age to the 20th century, with a special emphasis on the recurrence of three causal explanations for mental illness; supernatural, somatogenic, and psychogenic factors. This part briefly touches upon trephination, the Greek theory of hysteria within the context of the four bodily humors, witch hunts, asylums, moral treatment, mesmerism, catharsis, the mental hygiene movement, deinstitutionalization, community mental health services, and managed care. The third part concludes with a brief description of the issue of diagnosis.
Learning Objectives
- Identify what the criteria used to distinguish normality from abnormality are.
- Understand the difference among the three main etiological theories of mental illness.
- Describe specific beliefs or events in history that exemplify each of these etiological theories (e.g., hysteria, humorism, witch hunts, asylums, moral treatments).
- Explain the differences in treatment facilities for the mentally ill (e.g., mental hospitals, asylums, community mental health centers).
- Describe the features of the “moral treatment” approach used by Chiarughi, Pinel, and Tuke.
- Describe the reform efforts of Dix and Beers and the outcomes of their work.
- Describe Kräpelin’s classification of mental illness and the current DSM system.
History of Mental Illness
References to mental illness can be found throughout history. The evolution of mental illness, however, has not been linear or progressive but rather cyclical. Whether a behavior is considered normal or abnormal depends on the context surrounding the behavior and thus changes as a function of a particular time and culture. In the past, uncommon behavior or behavior that deviated from the sociocultural norms and expectations of a specific culture and period has been used as a way to silence or control certain individuals or groups. As a result, a less cultural relativist view of abnormal behavior has focused instead on whether behavior poses a threat to oneself or others or causes so much pain and suffering that it interferes with one’s work responsibilities or with one’s relationships with family and friends.
Throughout history there have been three general theories of the etiology of mental illness:supernatural, somatogenic, and psychogenic. Supernatural theories attribute mental illness to possession by evil or demonic spirits, displeasure of gods, eclipses, planetary gravitation, curses, and sin. Somatogenic theories identify disturbances in physical functioning resulting from either illness, genetic inheritance, or brain damage or imbalance. Psychogenic theories focus on traumatic or stressful experiences, maladaptive learned associations and cognitions, or distorted perceptions. Etiological theories of mental illness determine the care and treatment mentally ill individuals receive. As we will see below, an individual believed to be possessed by the devil will be viewed and treated differently from an individual believed to be suffering from an excess of yellow bile. Their treatments will also differ, from exorcism to blood-letting. The theories, however, remain the same. They coexist as well as recycle over time.
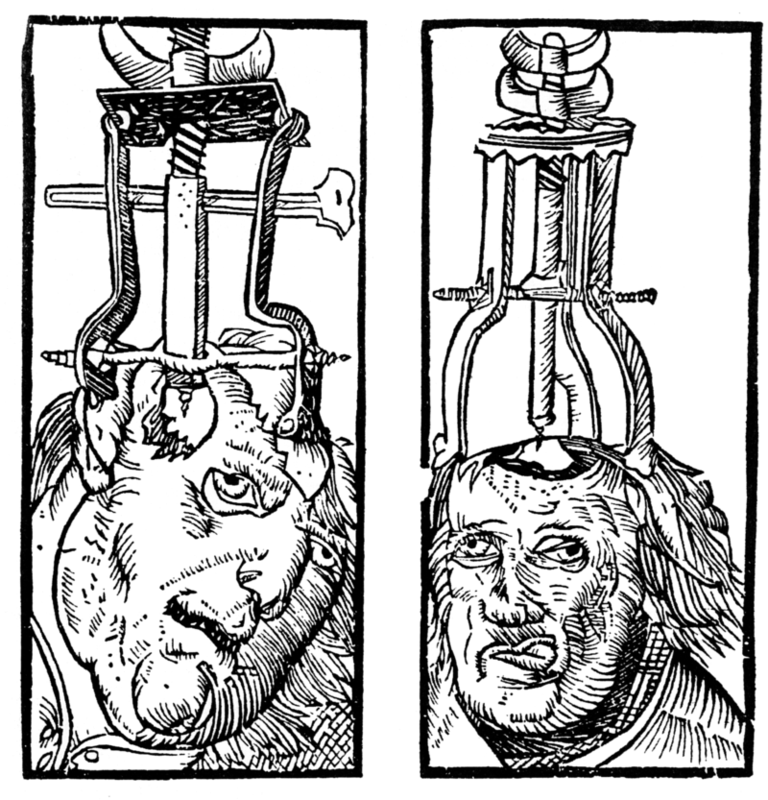
Trephination is an example of the earliest supernatural explanation for mental illness. Examination of prehistoric skulls and cave art from as early as 6500 BC has identified surgical drilling of holes in skulls to treat head injuries and epilepsy as well as to allow evil spirits trapped within the skull to be released (Restak, 2000). Around 2700 BC, Chinese medicine’s concept of complementary positive and negative bodily forces (“yin and yang”) attributed mental (and physical) illness to an imbalance between these forces. As such, a harmonious life that allowed for the proper balance of yin and yang and movement of vital air was essential (Tseng, 1973).
Mesopotamian and Egyptian papyri from 1900 BC describe women suffering from mental illness resulting from a wandering uterus (later named hysteria by the Greeks): The uterus could become dislodged and attached to parts of the body like the liver or chest cavity, preventing their proper functioning or producing varied and sometimes painful symptoms. As a result, the Egyptians, and later the Greeks, also employed a somatogenic treatment of strong smelling substances to guide the uterus back to its proper location (pleasant odors to lure and unpleasant ones to dispel).
Throughout classical antiquity we see a return to supernatural theories of demonic possession or godly displeasure to account for abnormal behavior that was beyond the person’s control. Temple attendance with religious healing ceremonies and incantations to the gods were employed to assist in the healing process. Hebrews saw madness as punishment from God, so treatment consisted of confessing sins and repenting. Physicians were also believed to be able to comfort and cure madness, however.
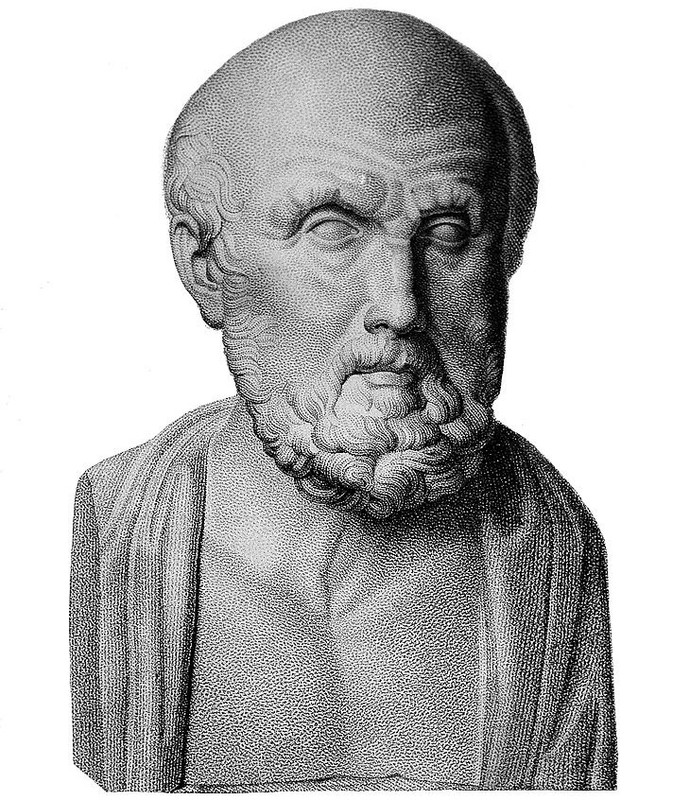
Greek physicians rejected supernatural explanations of mental disorders. It was around 400 BC that Hippocrates (460–370 BC) attempted to separate superstition and religion from medicine by systematizing the belief that a deficiency in or especially an excess of one of the four essential bodily fluids (i.e., humors)—blood, yellow bile, black bile, and phlegm—was responsible for physical and mental illness. For example, someone who was too temperamental suffered from too much blood and thus blood-letting would be the necessary treatment. Hippocrates classified mental illness into one of four categories—epilepsy, mania, melancholia, and brain fever—and like other prominent physicians and philosophers of his time, he did not believe mental illness was shameful or that mentally ill individuals should be held accountable for their behavior. Mentally ill individuals were cared for at home by family members and the state shared no responsibility for their care. Humorism remained a recurrent somatogenic theory up until the 19th century.
While Greek physician Galen (AD 130–201) rejected the notion of a uterus having an animistic soul, he agreed with the notion that an imbalance of the four bodily fluids could cause mental illness. He also opened the door for psychogenic explanations for mental illness, however, by allowing for the experience of psychological stress as a potential cause of abnormality. Galen’s psychogenic theories were ignored for centuries, however, as physicians attributed mental illness to physical causes throughout most of the millennium.
By the late Middle Ages, economic and political turmoil threatened the power of the Roman Catholic church. Between the 11th and 15th centuries, supernatural theories of mental disorders again dominated Europe, fueled by natural disasters like plagues and famines that lay people interpreted as brought about by the devil. Superstition, astrology, and alchemy took hold, and common treatments included prayer rites, relic touching, confessions, and atonement. Beginning in the 13th century the mentally ill, especially women, began to be persecuted as witches who were possessed. At the height of the witch hunts during the 15th through 17th centuries, with the Protestant Reformation having plunged Europe into religious strife, two Dominican monks wrote the Malleus Maleficarum (1486) as the ultimate manual to guide witch hunts. Johann Weyer and Reginald Scot tried to convince people in the mid- to late-16th century that accused witches were actually women with mental illnesses and that mental illness was not due to demonic possession but to faulty metabolism and disease, but the Church’s Inquisition banned both of their writings. Witch-hunting did not decline until the 17th and 18th centuries, after more than 100,000 presumed witches had been burned at the stake (Schoeneman, 1977; Zilboorg & Henry, 1941).
Modern treatments of mental illness are most associated with the establishment of hospitals and asylumsbeginning in the 16th century. Such institutions’ mission was to house and confine the mentally ill, the poor, the homeless, the unemployed, and the criminal. War and economic depression produced vast numbers of undesirables and these were separated from society and sent to these institutions. Two of the most well-known institutions, St. Mary of Bethlehem in London, known as Bedlam, and the Hôpital Général of Paris—which included La Salpêtrière, La Pitié, and La Bicêtre—began housing mentally ill patients in the mid-16th and 17th centuries. As confinement laws focused on protecting the public from the mentally ill, governments became responsible for housing and feeding undesirables in exchange for their personal liberty. Most inmates were institutionalized against their will, lived in filth and chained to walls, and were commonly exhibited to the public for a fee. Mental illness was nonetheless viewed somatogenically, so treatments were similar to those for physical illnesses: purges, bleedings, and emetics.
While inhumane by today’s standards, the view of insanity at the time likened the mentally ill to animals (i.e., animalism) who did not have the capacity to reason, could not control themselves, were capable of violence without provocation, did not have the same physical sensitivity to pain or temperature, and could live in miserable conditions without complaint. As such, instilling fear was believed to be the best way to restore a disordered mind to reason.
By the 18th century, protests rose over the conditions under which the mentally ill lived, and the 18th and 19th centuries saw the growth of a more humanitarian view of mental illness. In 1785 Italian physician Vincenzo Chiarughi (1759–1820) removed the chains of patients at his St. Boniface hospital in Florence, Italy, and encouraged good hygiene and recreational and occupational training. More well known, French physician Philippe Pinel (1745–1826) and former patient Jean-Baptise Pussin created a “traitement moral” at La Bicêtre and the Salpêtrière in 1793 and 1795 that also included unshackling patients, moving them to well-aired, well-lit rooms, and encouraging purposeful activity and freedom to move about the grounds (Micale, 1985).
In England, humanitarian reforms rose from religious concerns. William Tuke (1732–1822) urged the Yorkshire Society of (Quaker) Friends to establish the York Retreat in 1796, where patients were guests, not prisoners, and where the standard of care depended on dignity and courtesy as well as the therapeutic and moral value of physical work (Bell, 1980).

While America had asylums for the mentally ill—such as the Pennsylvania Hospital in Philadelphia and the Williamsburg Hospital, established in 1756 and 1773—the somatogenic theory of mental illness of the time—promoted especially by the father of America psychiatry, Benjamin Rush (1745–1813)—had led to treatments such as blood-letting, gyrators, and tranquilizer chairs. When Tuke’s York Retreat became the model for half of the new private asylums established in the United States, however, psychogenic treatments such as compassionate care and physical labor became the hallmarks of the new American asylums, such as the Friends Asylum in Frankford, Pennsylvania, and the Bloomingdale Asylum in New York City, established in 1817 and 1821 (Grob, 1994).
Moral treatment had to be abandoned in America in the second half of the 19th century, however, when these asylums became overcrowded and custodial in nature and could no longer provide the space nor attention necessary. When retired school teacher Dorothea Dix discovered the negligence that resulted from such conditions, she advocated for the establishment of state hospitals. Between 1840 and1880, she helped establish over 30 mental institutions in the United States and Canada (Viney & Zorich, 1982). By the late 19th century, moral treatment had given way to the mental hygiene movement, founded by former patient Clifford Beers with the publication of his 1908 memoir A Mind That Found Itself. Riding on Pasteur’s breakthrough germ theory of the 1860s and 1870s and especially on the early 20th century discoveries of vaccines for cholera, syphilis, and typhus, the mental hygiene movement reverted to a somatogenic theory of mental illness.
European psychiatry in the late 18th century and throughout the 19th century, however, struggled between somatogenic and psychogenic explanations of mental illness, particularly hysteria, which caused physical symptoms such as blindness or paralysis with no apparent physiological explanation. Franz Anton Mesmer (1734–1815), influenced by contemporary discoveries in electricity, attributed hysterical symptoms to imbalances in a universal magnetic fluid found in individuals, rather than to a wandering uterus (Forrest, 1999). James Braid (1795–1860) shifted this belief in mesmerism to one in hypnosis, thereby proposing a psychogenic treatment for the removal of symptoms. At the time, famed Salpetriere Hospital neurologist Jean-Martin Charcot (1825–1893), and Ambroise Auguste Liébault (1823–1904) and Hyppolyte Bernheim (1840–1919) of the Nancy School in France, were engaged in a bitter etiological battle over hysteria, with Charcot maintaining that the hypnotic suggestibility underlying hysteria was a neurological condition while Liébault and Bernheim believed it to be a general trait that varied in the population. Josef Breuer (1842–1925) and Sigmund Freud (1856–1939) would resolve this dispute in favor of a psychogenic explanation for mental illness by treating hysteria through hypnosis, which eventually led to the cathartic method that became the precursor for psychoanalysis during the first half of the 20th century.
Psychoanalysis was the dominant psychogenic treatment for mental illness during the first half of the 20th century, providing the launching pad for the more than 400 different schools of psychotherapy found today (Magnavita, 2006). Most of these schools cluster around broader behavioral, cognitive, cognitive-behavioral, psychodynamic, and client-centered approaches to psychotherapy applied in individual, marital, family, or group formats. Negligible differences have been found among all these approaches, however; their efficacy in treating mental illness is due to factors shared among all of the approaches (not particular elements specific to each approach): the therapist-patient alliance, the therapist’s allegiance to the therapy, therapist competence, and placebo effects (Luborsky et al., 2002; Messer & Wampold, 2002).
In contrast, the leading somatogenic treatment for mental illness can be found in the establishment of the first psychotropic medications in the mid-20th century. Restraints, electro-convulsive shock therapy, and lobotomies continued to be employed in American state institutions until the 1970s, but they quickly made way for a burgeoning pharmaceutical industry that has viewed and treated mental illness as a chemical imbalance in the brain.
Both etiological theories coexist today in what the psychological discipline holds as the biopsychosocial model of explaining human behavior. While individuals may be born with a genetic predisposition for a certain psychological disorder, certain psychological stressors need to be present for them to develop the disorder. Sociocultural factors such as sociopolitical or economic unrest, poor living conditions, or problematic interpersonal relationships are also viewed as contributing factors. However much we want to believe that we are above the treatments described above, or that the present is always the most enlightened time, let us not forget that our thinking today continues to reflect the same underlying somatogenic and psychogenic theories of mental illness discussed throughout this cursory 9,000-year history.
Diagnosis of Mental Illness
Progress in the treatment of mental illness necessarily implies improvements in the diagnosis of mental illness. A standardized diagnostic classification system with agreed-upon definitions of psychological disorders creates a shared language among mental-health providers and aids in clinical research. While diagnoses were recognized as far back as the Greeks, it was not until 1883 that German psychiatrist Emil Kräpelin (1856–1926) published a comprehensive system of psychological disorders that centered around a pattern of symptoms (i.e., syndrome) suggestive of an underlying physiological cause. Other clinicians also suggested popular classification systems but the need for a single, shared system paved the way for the American Psychiatric Association’s 1952 publication of the first Diagnostic and Statistical Manual (DSM).
The DSM has undergone various revisions (in 1968, 1980, 1987, 1994, 2000, 2013), and it is the 1980 DSM-III version that began a multiaxial classification system that took into account the entire individual rather than just the specific problem behavior. Axes I and II contain the clinical diagnoses, including mental retardation and personality disorders. Axes III and IV list any relevant medical conditions or psychosocial or environmental stressors, respectively. Axis V provides a global assessment of the individual’s level of functioning. The most recent version — the DSM-5– has combined the first three axes and removed the last two. These revisions reflect an attempt to help clinicians streamline diagnosis and work better with other diagnostic systems such as health diagnoses outlined by the World Health Organization.
While the DSM has provided a necessary shared language for clinicians, aided in clinical research, and allowed clinicians to be reimbursed by insurance companies for their services, it is not without criticism. The DSM is based on clinical and research findings from Western culture, primarily the United States. It is also a medicalized categorical classification system that assumes disordered behavior does not differ in degree but in kind, as opposed to a dimensional classification system that would plot disordered behavior along a continuum. Finally, the number of diagnosable disorders has tripled since it was first published in 1952, so that almost half of Americans will have a diagnosable disorder in their lifetime, contributing to the continued concern of labeling and stigmatizing mentally ill individuals. These concerns appear to be relevant even in the DSM-5 version that came out in May of 2013.
Therapeutic Orientations
By Hannah Boettcher, Stefan G. Hofmann, and Q. Jade Wu
Boston University
In the past century, a number of psychotherapeutic orientations have gained popularity for treating mental illnesses. This module outlines some of the best-known therapeutic approaches and explains the history, techniques, advantages, and disadvantages associated with each. The most effective modern approach is cognitive behavioral therapy (CBT). We also discuss psychoanalytic therapy, person-centered therapy, and mindfulness-based approaches. Drug therapy and emerging new treatment strategies will also be briefly explored.
Learning Objectives
- Become familiar with the most widely practiced approaches to psychotherapy.
- For each therapeutic approach, consider: history, goals, key techniques, and empirical support.
- Consider the impact of emerging treatment strategies in mental health.
Introduction
The history of mental illness can be traced as far back as 1500 BCE, when the ancient Egyptians noted cases of “distorted concentration” and “emotional distress in the heart or mind” (Nasser, 1987). Today, nearly half of all Americans will experience mental illness at some point in their lives, and mental health problems affect more than one-quarter of the population in any given year (Kessler et al., 2005). Fortunately, a range of psychotherapies exist to treat mental illnesses. This module provides an overview of some of the best-known schools of thought in psychotherapy. Currently, the most effective approach is called Cognitive Behavioral Therapy (CBT); however, other approaches, such as psychoanalytic therapy, person-centered therapy, and mindfulness-based therapies are also used—though the effectiveness of these treatments aren’t as clear as they are for CBT. Throughout this module, note the advantages and disadvantages of each approach, paying special attention to their support by empirical research.
Psychoanalysis and Psychodynamic Therapy
The earliest organized therapy for mental disorders was psychoanalysis. Made famous in the early 20th century by one of the best-known clinicians of all time, Sigmund Freud, this approach stresses that mental health problems are rooted in unconscious conflicts and desires. In order to resolve the mental illness, then, these unconscious struggles must be identified and addressed. Psychoanalysis often does this through exploring one’s early childhood experiences that may have continuing repercussions on one’s mental health in the present and later in life. Psychoanalysis is an intensive, long-term approach in which patients and therapists may meet multiple times per week, often for many years.
History of Psychoanalytic Therapy
Freud initially suggested that mental health problems arise from efforts to push inappropriate sexual urges out of conscious awareness (Freud, 1895/1955). Later, Freud suggested more generally that psychiatric problems are the result of tension between different parts of the mind: the id, the superego, and the ego. In Freud’s structural model, the id represents pleasure-driven unconscious urges (e.g., our animalistic desires for sex and aggression), while the superego is the semi-conscious part of the mind where morals and societal judgment are internalized (e.g., the part of you that automatically knows how society expects you to behave). The ego—also partly conscious—mediates between the id and superego. Freud believed that bringing unconscious struggles like these (where the id demands one thing and the superego another) into conscious awareness would relieve the stress of the conflict (Freud, 1920/1955)—which became the goal of psychoanalytic therapy.
Although psychoanalysis is still practiced today, it has largely been replaced by the more broadly defined psychodynamic therapy. This latter approach has the same basic tenets as psychoanalysis, but is briefer, makes more of an effort to put clients in their social and interpersonal context, and focuses more on relieving psychological distress than on changing the person.
Techniques in Psychoanalysis
Psychoanalysts and psychodynamic therapists employ several techniques to explore patients’ unconscious mind. One common technique is called free association. Here, the patient shares any and all thoughts that come to mind, without attempting to organize or censor them in any way. For example, if you took a pen and paper and just wrote down whatever came into your head, letting one thought lead to the next without allowing conscious criticism to shape what you were writing, you would be doing free association. The analyst then uses his or her expertise to discern patterns or underlying meaning in the patient’s thoughts.
Sometimes, free association exercises are applied specifically to childhood recollections. That is, psychoanalysts believe a person’s childhood relationships with caregivers often determine the way that person relates to others, and predicts later psychiatric difficulties. Thus, exploring these childhood memories, through free association or otherwise, can provide therapists with insights into a patient’s psychological makeup.
Because we don’t always have the ability to consciously recall these deep memories, psychoanalysts also discuss their patients’ dreams. In Freudian theory, dreams contain not only manifest (or literal) content, but also latent (or symbolic) content (Freud, 1900; 1955). For example, someone may have a dream that his/her teeth are falling out—the manifest or actual content of the dream. However, dreaming that one’s teeth are falling out could be a reflection of the person’s unconscious concern about losing his or her physical attractiveness—the latent or metaphorical content of the dream. It is the therapist’s job to help discover the latent content underlying one’s manifest content through dream analysis.
In psychoanalytic and psychodynamic therapy, the therapist plays a receptive role—interpreting the patient’s thoughts and behavior based on clinical experience and psychoanalytic theory. For example, if during therapy a patient begins to express unjustified anger toward the therapist, the therapist may recognize this as an act of transference. That is, the patient may be displacing feelings for people in his or her life (e.g., anger toward a parent) onto the therapist. At the same time, though, the therapist has to be aware of his or her own thoughts and emotions, for, in a related process, called countertransference, the therapist may displace his/her own emotions onto the patient.
The key to psychoanalytic theory is to have patients uncover the buried, conflicting content of their mind, and therapists use various tactics—such as seating patients to face away from them—to promote a freer self-disclosure. And, as a therapist spends more time with a patient, the therapist can come to view his or her relationship with the patient as another reflection of the patient’s mind.
Advantages and Disadvantages of Psychoanalytic Therapy
Psychoanalysis was once the only type of psychotherapy available, but presently the number of therapists practicing this approach is decreasing around the world. Psychoanalysis is not appropriate for some types of patients, including those with severe psychopathology or mental retardation. Further, psychoanalysis is often expensive because treatment usually lasts many years. Still, some patients and therapists find the prolonged and detailed analysis very rewarding.
Perhaps the greatest disadvantage of psychoanalysis and related approaches is the lack of empirical support for their effectiveness. The limited research that has been conducted on these treatments suggests that they do not reliably lead to better mental health outcomes (e.g., Driessen et al., 2010). And, although there are some reviews that seem to indicate that long-term psychodynamic therapies might be beneficial (e.g., Leichsenring & Rabung, 2008), other researchers have questioned the validity of these reviews. Nevertheless, psychoanalytic theory was history’s first attempt at formal treatment of mental illness, setting the stage for the more modern approaches used today.
Humanistic and Person-Centered Therapy
One of the next developments in therapy for mental illness, which arrived in the mid-20th century, is called humanistic or person-centered therapy (PCT). Here, the belief is that mental health problems result from an inconsistency between patients’ behavior and their true personal identity. Thus, the goal of PCT is to create conditions under which patients can discover their self-worth, feel comfortable exploring their own identity, and alter their behavior to better reflect this identity.
History of Person-Centered Therapy

PCT was developed by a psychologist named Carl Rogers, during a time of significant growth in the movements of humanistic theory and human potential. These perspectives were based on the idea that humans have an inherent drive to realize and express their own capabilities and creativity. Rogers, in particular, believed that all people have the potential to change and improve, and that the role of therapists is to foster self-understanding in an environment where adaptive change is most likely to occur (Rogers, 1951). Rogers suggested that the therapist and patient must engage in a genuine, egalitarian relationship in which the therapist is nonjudgmental and empathetic. In PCT, the patient should experience both a vulnerability to anxiety, which motivates the desire to change, and an appreciation for the therapist’s support.
Techniques in Person-Centered Therapy
Humanistic and person-centered therapy, like psychoanalysis, involves a largely unstructured conversation between the therapist and the patient. Unlike psychoanalysis, though, a therapist using PCT takes a passive role, guiding the patient toward his or her own self-discovery. Rogers’s original name for PCT was non-directive therapy, and this notion is reflected in the flexibility found in PCT. Therapists do not try to change patients’ thoughts or behaviors directly. Rather, their role is to provide the therapeutic relationship as a platform for personal growth. In these kinds of sessions, the therapist tends only to ask questions and doesn’t provide any judgment or interpretation of what the patient says. Instead, the therapist is present to provide a safe and encouraging environment for the person to explore these issues for him- or herself.
An important aspect of the PCT relationship is the therapist’s unconditional positive regard for the patient’s feelings and behaviors. That is, the therapist is never to condemn or criticize the patient for what s/he has done or thought; the therapist is only to express warmth and empathy. This creates an environment free of approval or disapproval, where patients come to appreciate their value and to behave in ways that are congruent with their own identity.
Advantages and Disadvantages of Person-Centered Therapy
One key advantage of person-centered therapy is that it is highly acceptable to patients. In other words, people tend to find the supportive, flexible environment of this approach very rewarding. Furthermore, some of the themes of PCT translate well to other therapeutic approaches. For example, most therapists of any orientation find that clients respond well to being treated with nonjudgmental empathy. The main disadvantage to PCT, however, is that findings about its effectiveness are mixed. One possibility for this could be that the treatment is primarily based on unspecific treatment factors. That is, rather than using therapeutic techniques that are specific to the patient and the mental problem (i.e., specific treatment factors), the therapy focuses on techniques that can be applied to anyone (e.g., establishing a good relationship with the patient) (Cuijpers et al., 2012; Friedli, King, Lloyd, & Horder, 1997). Similar to how “one-size-fits-all” doesn’t really fit every person, PCT uses the same practices for everyone, which may work for some people but not others. Further research is necessary to evaluate its utility as a therapeutic approach.
Cognitive Behavioral Therapy
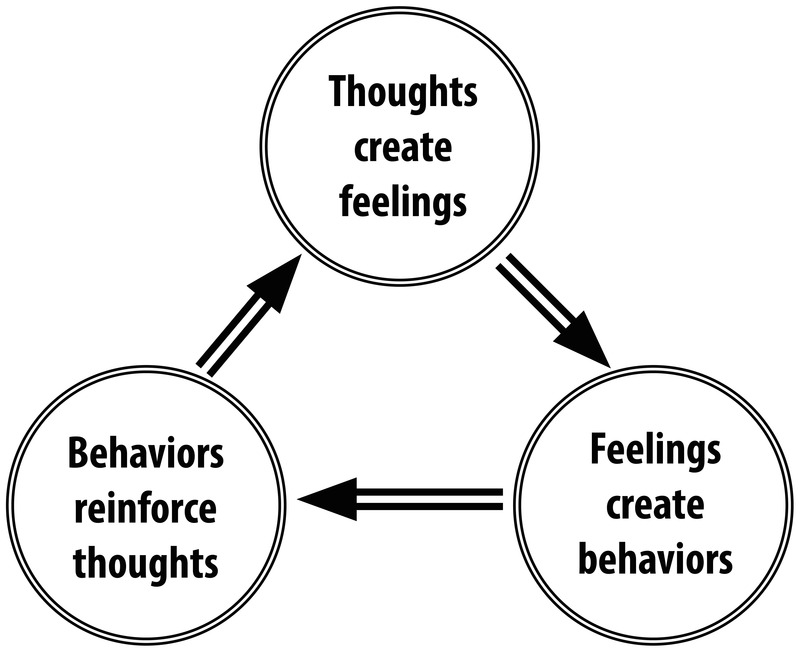
Although both psychoanalysis and PCT are still used today, another therapy, cognitive-behavioral therapy (CBT), has gained more widespread support and practice. CBT refers to a family of therapeutic approaches whose goal is to alleviate psychological symptoms by changing their underlying cognitions and behaviors. The premise of CBT is that thoughts, behaviors, and emotions interact and contribute to various mental disorders. For example, let’s consider how a CBT therapist would view a patient who compulsively washes her hands for hours every day. First, the therapist would identify the patient’s maladaptive thought: “If I don’t wash my hands like this, I will get a disease and die.” The therapist then identifies how this maladaptive thought leads to a maladaptive emotion: the feeling of anxiety when her hands aren’t being washed. And finally, this maladaptive emotion leads to the maladaptive behavior: the patient washing her hands for hours every day.
CBT is a present-focused therapy (i.e., focused on the “now” rather than causes from the past, such as childhood relationships) that uses behavioral goals to improve one’s mental illness. Often, these behavioral goals involve between-session homework assignments. For example, the therapist may give the hand-washing patient a worksheet to take home; on this worksheet, the woman is to write down every time she feels the urge to wash her hands, how she deals with the urge, and what behavior she replaces that urge with. When the patient has her next therapy session, she and the therapist review her “homework” together. CBT is a relatively brief intervention of 12 to 16 weekly sessions, closely tailored to the nature of the psychopathology and treatment of the specific mental disorder. And, as the empirical data shows, CBT has proven to be highly efficacious for virtually all psychiatric illnesses (Hofmann, Asnaani, Vonk, Sawyer, & Fang, 2012).
History of Cognitive Behavioral Therapy
CBT developed from clinical work conducted in the mid-20th century by Dr. Aaron T. Beck, a psychiatrist, and Albert Ellis, a psychologist. Beck used the term automatic thoughts to refer to the thoughts depressed patients report experiencing spontaneously. He observed that these thoughts arise from three belief systems, or schemas: beliefs about the self, beliefs about the world, and beliefs about the future. In treatment, therapy initially focuses on identifying automatic thoughts (e.g., “If I don’t wash my hands constantly, I’ll get a disease”), testing their validity, and replacing maladaptive thoughts with more adaptive thoughts (e.g., “Washing my hands three times a day is sufficient to prevent a disease”). In later stages of treatment, the patient’s maladaptive schemas are examined and modified. Ellis (1957) took a comparable approach, in what he called rational-emotive-behavioral therapy (REBT), which also encourages patients to evaluate their own thoughts about situations.
Techniques in CBT
Beck and Ellis strove to help patients identify maladaptive appraisals, or the untrue judgments and evaluations of certain thoughts. For example, if it’s your first time meeting new people, you may have the automatic thought, “These people won’t like me because I have nothing interesting to share.” That thought itself is not what’s troublesome; the appraisal (or evaluation) that it might have merit is what’s troublesome. The goal of CBT is to help people make adaptive, instead of maladaptive, appraisals (e.g., “I do know interesting things!”). This technique of reappraisal, or cognitive restructuring, is a fundamental aspect of CBT. With cognitive restructuring, it is the therapist’s job to help point out when a person has an inaccurate or maladaptive thought, so that the patient can either eliminate it or modify it to be more adaptive.
In addition to thoughts, though, another important treatment target of CBT is maladaptive behavior. Every time a person engages in maladaptive behavior (e.g., never speaking to someone in new situations), he or she reinforces the validity of the maladaptive thought, thus maintaining or perpetuating the psychological illness. In treatment, the therapist and patient work together to develop healthy behavioral habits (often tracked with worksheet-like homework), so that the patient can break this cycle of maladaptive thoughts and behaviors.
For many mental health problems, especially anxiety disorders, CBT incorporates what is known as exposure therapy. During exposure therapy, a patient confronts a problematic situation and fully engages in the experience instead of avoiding it. For example, imagine a man who is terrified of spiders. Whenever he encounters one, he immediately screams and panics. In exposure therapy, the man would be forced to confront and interact with spiders, rather than simply avoiding them as he usually does. The goal is to reduce the fear associated with the situation through extinction learning, a neurobiological and cognitive process by which the patient “unlearns” the irrational fear. For example, exposure therapy for someone terrified of spiders might begin with him looking at a cartoon of a spider, followed by him looking at pictures of real spiders, and later, him handling a plastic spider. After weeks of this incremental exposure, the patient may even be able to hold a live spider. After repeated exposure (starting small and building one’s way up), the patient experiences less physiological fear and maladaptive thoughts about spiders, breaking his tendency for anxiety and subsequent avoidance.
Advantages and Disadvantages of CBT
CBT interventions tend to be relatively brief, making them cost-effective for the average consumer. In addition, CBT is an intuitive treatment that makes logical sense to patients. It can also be adapted to suit the needs of many different populations. One disadvantage, however, is that CBT does involve significant effort on the patient’s part, because the patient is an active participant in treatment. Therapists often assign “homework” (e.g., worksheets for recording one’s thoughts and behaviors) between sessions to maintain the cognitive and behavioral habits the patient is working on. The greatest strength of CBT is the abundance of empirical support for its effectiveness. Studies have consistently found CBT to be equally or more effective than other forms of treatment, including medication and other therapies (Butler, Chapman, Forman, & Beck, 2006; Hofmann et al., 2012). For this reason, CBT is considered a first-line treatment for many mental disorders.
The central notion of CBT is the idea that a person’s behavioral and emotional responses are causally influenced by one’s thinking. The stoic Greek philosopher Epictetus is quoted as saying, “men are not moved by things, but by the view they take of them.” Meaning, it is not the event per se, but rather one’s assumptions (including interpretations and perceptions) of the event that are responsible for one’s emotional response to it. Beck calls these assumptions about events and situations automatic thoughts (Beck, 1979), whereas Ellis (1962) refers to these assumptions as self-statements. The cognitive model assumes that these cognitive processes cause the emotional and behavioral responses to events or stimuli. This causal chain is illustrated in Ellis’s ABC model, in which A stands for the antecedent event, B stands for belief, and C stands for consequence. During CBT, the person is encouraged to carefully observe the sequence of events and the response to them, and then explore the validity of the underlying beliefs through behavioral experiments and reasoning, much like a detective or scientist.
Acceptance and Mindfulness-Based Approaches
Unlike the preceding therapies, which were developed in the 20th century, this next one was born out of age-old Buddhist and yoga practices. Mindfulness, or a process that tries to cultivate a nonjudgmental, yet attentive, mental state, is a therapy that focuses on one’s awareness of bodily sensations, thoughts, and the outside environment. Whereas other therapies work to modify or eliminate these sensations and thoughts, mindfulness focuses on nonjudgmentally accepting them (Kabat-Zinn, 2003; Baer, 2003). For example, whereas CBT may actively confront and work to change a maladaptive thought, mindfulness therapy works to acknowledge and accept the thought, understanding that the thought is spontaneous and not what the person truly believes. There are two important components of mindfulness: (1) self-regulation of attention, and (2) orientation toward the present moment (Bishop et al., 2004). Mindfulness is thought to improve mental health because it draws attention away from past and future stressors, encourages acceptance of troubling thoughts and feelings, and promotes physical relaxation.
Techniques in Mindfulness-Based Therapy
Psychologists have adapted the practice of mindfulness as a form of psychotherapy, generally called mindfulness-based therapy (MBT). Several types of MBT have become popular in recent years, including mindfulness-based stress reduction (MBSR) (e.g., Kabat-Zinn, 1982) and mindfulness-based cognitive therapy (MBCT) (e.g., Segal, Williams, & Teasdale, 2002).

MBSR uses meditation, yoga, and attention to physical experiences to reduce stress. The hope is that reducing a person’s overall stress will allow that person to more objectively evaluate his or her thoughts. In MBCT, rather than reducing one’s general stress to address a specific problem, attention is focused on one’s thoughts and their associated emotions. For example, MBCT helps prevent relapses in depression by encouraging patients to evaluate their own thoughts objectively and without value judgment (Baer, 2003). Although cognitive behavioral therapy (CBT) may seem similar to this, it focuses on “pushing out” the maladaptive thought, whereas mindfulness-based cognitive therapy focuses on “not getting caught up” in it. The treatments used in MBCT have been used to address a wide range of illnesses, including depression, anxiety, chronic pain, coronary artery disease, and fibromyalgia (Hofmann, Sawyer, Witt & Oh, 2010).
Mindfulness and acceptance—in addition to being therapies in their own right—have also been used as “tools” in other cognitive-behavioral therapies, particularly in dialectical behavior therapy (DBT) (e.g., Linehan, Amstrong, Suarez, Allmon, & Heard, 1991). DBT, often used in the treatment of borderline personality disorder, focuses on skills training. That is, it often employs mindfulness and cognitive behavioral therapy practices, but it also works to teach its patients “skills” they can use to correct maladaptive tendencies. For example, one skill DBT teaches patients is called distress tolerance—or, ways to cope with maladaptive thoughts and emotions in the moment. For example, people who feel an urge to cut themselves may be taught to snap their arm with a rubber band instead. The primary difference between DBT and CBT is that DBT employs techniques that address the symptoms of the problem (e.g., cutting oneself) rather than the problem itself (e.g., understanding the psychological motivation to cut oneself). CBT does not teach such skills training because of the concern that the skills—even though they may help in the short-term—may be harmful in the long-term, by maintaining maladaptive thoughts and behaviors.
DBT is founded on the perspective of a dialectical worldview. That is, rather than thinking of the world as “black and white,” or “only good and only bad,” it focuses on accepting that some things can have characteristics of both “good” and “bad.” So, in a case involving maladaptive thoughts, instead of teaching that a thought is entirely bad, DBT tries to help patients be less judgmental of their thoughts (as with mindfulness-based therapy) and encourages change through therapeutic progress, using cognitive-behavioral techniques as well as mindfulness exercises.
Another form of treatment that also uses mindfulness techniques is acceptance and commitment therapy (ACT) (Hayes, Strosahl, & Wilson, 1999). In this treatment, patients are taught to observe their thoughts from a detached perspective (Hayes et al., 1999). ACT encourages patients not to attempt to change or avoid thoughts and emotions they observe in themselves, but to recognize which are beneficial and which are harmful. However, the differences among ACT, CBT, and other mindfulness-based treatments are a topic of controversy in the current literature.
Advantages and Disadvantages of Mindfulness-Based Therapy
Two key advantages of mindfulness-based therapies are their acceptability and accessibility to patients. Because yoga and meditation are already widely known in popular culture, consumers of mental healthcare are often interested in trying related psychological therapies. Currently, psychologists have not come to a consensus on the efficacy of MBT, though growing evidence supports its effectiveness for treating mood and anxiety disorders. For example, one review of MBT studies for anxiety and depression found that mindfulness-based interventions generally led to moderate symptom improvement (Hofmann et al., 2010).
Emerging Treatment Strategies

With growth in research and technology, psychologists have been able to develop new treatment strategies in recent years. Often, these approaches focus on enhancing existing treatments, such as cognitive-behavioral therapies, through the use of technological advances. For example, internet- and mobile-delivered therapies make psychological treatments more available, through smartphones and online access. Clinician-supervised online CBT modules allow patients to access treatment from home on their own schedule—an opportunity particularly important for patients with less geographic or socioeconomic access to traditional treatments. Furthermore, smartphones help extend therapy to patients’ daily lives, allowing for symptom tracking, homework reminders, and more frequent therapist contact.
Another benefit of technology is cognitive bias modification. Here, patients are given exercises, often through the use of video games, aimed at changing their problematic thought processes. For example, researchers might use a mobile app to train alcohol abusers to avoid stimuli related to alcohol. One version of this game flashes four pictures on the screen—three alcohol cues (e.g., a can of beer, the front of a bar) and one health-related image (e.g., someone drinking water). The goal is for the patient to tap the healthy picture as fast as s/he can. Games like these aim to target patients’ automatic, subconscious thoughts that may be difficult to direct through conscious effort. That is, by repeatedly tapping the healthy image, the patient learns to “ignore” the alcohol cues, so when those cues are encountered in the environment, they will be less likely to trigger the urge to drink. Approaches like these are promising because of their accessibility, however they require further research to establish their effectiveness.
Yet another emerging treatment employs CBT-enhancing pharmaceutical agents. These are drugs used to improve the effects of therapeutic interventions. Based on research from animal experiments, researchers have found that certain drugs influence the biological processes known to be involved in learning. Thus, if people take these drugs while going through psychotherapy, they are better able to “learn” the techniques for improvement. For example, the antibiotic d-cycloserine improves treatment for anxiety disorders by facilitating the learning processes that occur during exposure therapy. Ongoing research in this exciting area may prove to be quite fruitful.
Pharmacological Treatments
Up until this point, all the therapies we have discussed have been talk-based or meditative practices. However, psychiatric medications are also frequently used to treat mental disorders, including schizophrenia, bipolar disorder, depression, and anxiety disorders. Psychiatric drugs are commonly used, in part, because they can be prescribed by general medical practitioners, whereas only trained psychologists are qualified to deliver effective psychotherapy. While drugs and CBT therapies tend to be almost equally effective, choosing the best intervention depends on the disorder and individual being treated, as well as other factors—such as treatment availability and comorbidity (i.e., having multiple mental or physical disorders at once). Although many new drugs have been introduced in recent decades, there is still much we do not understand about their mechanism in the brain. Further research is needed to refine our understanding of both pharmacological and behavioral treatments before we can make firm claims about their effectiveness.
Integrative and Eclectic Psychotherapy
In discussing therapeutic orientations, it is important to note that some clinicians incorporate techniques from multiple approaches, a practice known as integrative or eclectic psychotherapy. For example, a therapist may employ distress tolerance skills from DBT (to resolve short-term problems), cognitive reappraisal from CBT (to address long-standing issues), and mindfulness-based meditation from MBCT (to reduce overall stress). And, in fact, between 13% and 42% of therapists have identified their own approaches as integrative or eclectic (Norcross & Goldfried, 2005).
Conclusion
Throughout human history we have had to deal with mental illness in one form or another. Over time, several schools of thought have emerged for treating these problems. Although various therapies have been shown to work for specific individuals, cognitive behavioral therapy is currently the treatment most widely supported by empirical research. Still, practices like psychodynamic therapies, person-centered therapy, mindfulness-based treatments, and acceptance and commitment therapy have also shown success. And, with recent advances in research and technology, clinicians are able to enhance these and other therapies to treat more patients more effectively than ever before. However, what is important in the end is that people actually seek out mental health specialists to help them with their problems. One of the biggest deterrents to doing so is that people don’t understand what psychotherapy really entails. Through understanding how current practices work, not only can we better educate people about how to get the help they need, but we can continue to advance our treatments to be more effective in the future.
Outside Resources
- Video: An introduction to and overview of psychology, from its origins in the nineteenth century to current study of the brain’s biochemistry.
- http://www.learner.org/series/discoveringpsychology/01/e01expand.html
- Video: The BBC provides an overview of ancient Greek approaches to health and medicine.
- https://www.tes.com/teaching-resource/ancient-greek-approaches-to-health-and-medicine-6176019
- Web: Images from the History of Medicine. Search \”mental illness\”
- http://ihm.nlm.nih.gov/luna/servlet/view/all
- Web: Science Museum Brought to Life
- http://www.sciencemuseum.org.uk/broughttolife/themes/menalhealthandillness.aspx
- Web: The Social Psychology Network provides a number of links and resources.
- https://www.socialpsychology.org/history.htm
- Web: The UCL Center for the History of Medicine
- http://www.ucl.ac.uk/histmed/
- Web: The Wellcome Library. Search \”mental illness\”.
- http://wellcomelibrary.org/
- Web: US National Library of Medicine
- http://vsearch.nlm.nih.gov/vivisimo/cgi-bin/query-meta?query=mental+illness&v:project=nlm-main-website
- Article: A personal account of the benefits of mindfulness-based therapy
- https://www.theguardian.com/lifeandstyle/2014/jan/11/julie-myerson-mindfulness-based-cognitive-therapy
- Article: The Effect of Mindfulness-Based Therapy on Anxiety and Depression: A Meta-Analytic Review
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2848393/
- Web: An overview of the purpose and practice of cognitive behavioral therapy (CBT)
- http://psychcentral.com/lib/in-depth-cognitive-behavioral-therapy/
- Web: The history and development of psychoanalysis
- http://www.freudfile.org/psychoanalysis/history.html
Discussion Questions
- What does it mean to say that someone is mentally ill? What criteria are usually considered to determine whether someone is mentally ill?
- Describe the difference between supernatural, somatogenic, and psychogenic theories of mental illness and how subscribing to a particular etiological theory determines the type of treatment used.
- How did the Greeks describe hysteria and what treatment did they prescribe?
- Describe humorism and how it explained mental illness.
- Describe how the witch hunts came about and their relationship to mental illness.
- Describe the development of treatment facilities for the mentally insane, from asylums to community mental health centers.
- Describe the humane treatment of the mentally ill brought about by Chiarughi, Pinel, and Tuke in the late 18th and early 19th centuries and how it differed from the care provided in the centuries preceding it.
- Describe William Tuke’s treatment of the mentally ill at the York Retreat within the context of the Quaker Society of Friends. What influence did Tuke’s treatment have in other parts of the world?
- What are the 20th-century treatments resulting from the psychogenic and somatogenic theories of mental illness?
- Describe why a classification system is important and how the leading classification system used in the United States works. Describe some concerns with regard to this system.
- Psychoanalytic theory is no longer the dominant therapeutic approach, because it lacks empirical support. Yet many consumers continue to seek psychoanalytic or psychodynamic treatments. Do you think psychoanalysis still has a place in mental health treatment? If so, why?
- What might be some advantages and disadvantages of technological advances in psychological treatment? What will psychotherapy look like 100 years from now?
- Some people have argued that all therapies are about equally effective, and that they all affect change through common factors such as the involvement of a supportive therapist. Does this claim sound reasonable to you? Why or why not?
- When choosing a psychological treatment for a specific patient, what factors besides the treatment’s demonstrated efficacy should be taken into account?
Vocabulary
- Animism
- The belief that everyone and everything had a “soul” and that mental illness was due to animistic causes, for example, evil spirits controlling an individual and his/her behavior.
- Asylum
- A place of refuge or safety established to confine and care for the mentally ill; forerunners of the mental hospital or psychiatric facility.
- A model in which the interaction of biological, psychological, and sociocultural factors is seen as influencing the development of the individual.
- Cathartic method
- A therapeutic procedure introduced by Breuer and developed further by Freud in the late 19th century whereby a patient gains insight and emotional relief from recalling and reliving traumatic events.
- Cultural relativism
- The idea that cultural norms and values of a society can only be understood on their own terms or in their own context.
- Etiology
- The causal description of all of the factors that contribute to the development of a disorder or illness.
- Humorism (or humoralism)
- A belief held by ancient Greek and Roman physicians (and until the 19th century) that an excess or deficiency in any of the four bodily fluids, or humors—blood, black bile, yellow bile, and phlegm—directly affected their health and temperament.
- Hysteria
- Term used by the ancient Greeks and Egyptians to describe a disorder believed to be caused by a woman’s uterus wandering throughout the body and interfering with other organs (today referred to as conversion disorder, in which psychological problems are expressed in physical form).
- Maladaptive
- Term referring to behaviors that cause people who have them physical or emotional harm, prevent them from functioning in daily life, and/or indicate that they have lost touch with reality and/or cannot control their thoughts and behavior (also called dysfunctional).
- Mesmerism
- Derived from Franz Anton Mesmer in the late 18th century, an early version of hypnotism in which Mesmer claimed that hysterical symptoms could be treated through animal magnetism emanating from Mesmer’s body and permeating the universe (and later through magnets); later explained in terms of high suggestibility in individuals.
- Psychogenesis
- Developing from psychological origins.
- Somatogenesis
- Developing from physical/bodily origins.
- Supernatural
- Developing from origins beyond the visible observable universe.
- Syndrome
- Involving a particular group of signs and symptoms.
- “Traitement moral” (moral treatment)
- A therapeutic regimen of improved nutrition, living conditions, and rewards for productive behavior that has been attributed to Philippe Pinel during the French Revolution, when he released mentally ill patients from their restraints and treated them with compassion and dignity rather than with contempt and denigration.
- Trephination
- The drilling of a hole in the skull, presumably as a way of treating psychological disorders.
- Acceptance and commitment therapy
- A therapeutic approach designed to foster nonjudgmental observation of one’s own mental processes.
- Automatic thoughts
- Thoughts that occur spontaneously; often used to describe problematic thoughts that maintain mental disorders.
- Cognitive bias modification
- Using exercises (e.g., computer games) to change problematic thinking habits.
- Cognitive-behavioral therapy (CBT)
- A family of approaches with the goal of changing the thoughts and behaviors that influence psychopathology.
- Comorbidity
- Describes a state of having more than one psychological or physical disorder at a given time.
- Dialectical behavior therapy (DBT)
- A treatment often used for borderline personality disorder that incorporates both cognitive-behavioral and mindfulness elements.
- Dialectical worldview
- A perspective in DBT that emphasizes the joint importance of change and acceptance.
- Exposure therapy
- A form of intervention in which the patient engages with a problematic (usually feared) situation without avoidance or escape.
- Free association
- In psychodynamic therapy, a process in which the patient reports all thoughts that come to mind without censorship, and these thoughts are interpreted by the therapist.
- Integrative or eclectic psychotherapy
- Also called integrative psychotherapy, this term refers to approaches combining multiple orientations (e.g., CBT with psychoanalytic elements).
- Integrative or eclectic psychotherapy
- Also called integrative psychotherapy, this term refers to approaches combining multiple orientations (e.g., CBT with psychoanalytic elements).
- Mindfulness
- A process that reflects a nonjudgmental, yet attentive, mental state.
- Mindfulness-based therapy
- A form of psychotherapy grounded in mindfulness theory and practice, often involving meditation, yoga, body scan, and other features of mindfulness exercises.
- Person-centered therapy
- A therapeutic approach focused on creating a supportive environment for self-discovery.
- Psychoanalytic therapy
- Sigmund Freud’s therapeutic approach focusing on resolving unconscious conflicts.
- Psychodynamic therapy
- Treatment applying psychoanalytic principles in a briefer, more individualized format.
- Reappraisal, or Cognitive restructuring
- The process of identifying, evaluating, and changing maladaptive thoughts in psychotherapy.
- Schema
- A mental representation or set of beliefs about something.
- Unconditional positive regard
- In person-centered therapy, an attitude of warmth, empathy and acceptance adopted by the therapist in order to foster feelings of inherent worth in the patient.
References
- Bell, L. V. (1980). Treating the mentally ill: From colonial times to the present. New York: Praeger.
- Forrest, D. (1999). Hypnotism: A history. New York: Penguin.
- Grob, G. N. (1994). The mad among us: A history of the care of America’s mentally ill. New York: Free Press.
- Luborsky, L., Rosenthal, R., Diguer, L., Andrusyna, T. P., Berman, J. S., Levitt, J. T., . . . Krause, E. D. (2002). The dodo bird verdict is alive and well—mostly. Clinical Psychology: Science and Practice, 9, 2–12.
- Messer, S. B., & Wampold, B. E. (2002). Let’s face facts: Common factors are more potent than specific therapy ingredients. Clinical Psychology: Science and Practice, 9(1), 21–25.
- Micale, M. S. (1985). The Salpêtrière in the age of Charcot: An institutional perspective on medical history in the late nineteenth century. Journal of Contemporary History, 20, 703–731.
- Restak, R. (2000). Mysteries of the mind. Washington, DC: National Geographic Society.
- Schoeneman, T. J. (1977). The role of mental illness in the European witch hunts of the sixteenth and seventeenth centuries: An assessment. Journal of the History of the Behavioral Sciences, 13(4), 337–351.
- Tseng, W. (1973). The development of psychiatric concepts in traditional Chinese medicine. Archives of General Psychiatry, 29, 569–575.
- Viney, W., & Zorich, S. (1982). Contributions to the history of psychology: XXIX. Dorothea Dix and the history of psychology. Psychological Reports, 50, 211–218.
- Zilboorg, G., & Henry, G. W. (1941). A history of medical psychology. New York: W. W. Norton.
- Baer, R. (2003). Mindfulness training as a clinical intervention: A conceptual and empirical review. Clinical Psychology: Science and Practice, 10, 125–143.
- Beck, A. T. (1979). Cognitive therapy and the emotional disorders. New York, NY: New American Library/Meridian.
- Bishop, S. R., Lau, M., Shapiro, S., Carlson, L., Anderson, N. D., Carmody, J., Segal, Z. V., Abbey, S., Speca, M., Velting, D., & Devins, G. (2004). Mindfulness: A proposed operational definition. Clinical Psychology: Science and Practice, 11, 230–241.
- Butler, A. C., Chapman, J. E., Forman, E. M., & Beck, A. T. (2006). The empirical status of cognitive behavioral therapy: A review of meta-analyses. Clinical Psychology Review, 26, 17–31.
- Cuijpers, P., Driessen, E., Hollon, S.D., van Oppen, P., Barth, J., & Andersson, G. (2012). The efficacy of non-directive supportive therapy for adult depression: A meta-analysis. Clinical Psychology Review, 32, 280–291.
- Driessen, E., Cuijpers, P., de Maat, S. C. M., Abbass, A. A., de Jonghe, F., & Dekker, J. J. M. (2010). The efficacy of short-term psychodynamic psychotherapy for depression: A meta-analysis. Clinical Psychology Review, 30, 25–36.
- Ellis, A. (1962). Reason and emotion in psychotherapy. New York, NY: Lyle Stuart.
- Ellis, A. (1957). Rational psychotherapy and individual psychology. Journal of Individual Psychology, 13, 38–44.
- Freud, S. (1955). The interpretation of dreams. London, UK: Hogarth Press (Original work published 1900).
- Freud, S. (1955). Studies on hysteria. London, UK: Hogarth Press (Original work published 1895).
- Freud. S. (1955). Beyond the pleasure principle. H London, UK: Hogarth Press (Original work published 1920).
- Friedli, K., King, M. B., Lloyd, M., & Horder, J. (1997). Randomized controlled assessment of non-directive psychotherapy versus routine general-practitioner care. Lancet, 350,\\n1662–1665.
- Hayes, S. C., Strosahl, K., & Wilson, K. G. (1999). Acceptance and Commitment Therapy. New\\nYork, NY: Guilford Press.
- Hofmann, S. G., Asnaani, A., Vonk, J. J., Sawyer, A. T., & Fang, A. (2012). The efficacy of cognitive behavioral therapy: A review of meta-analyses. Cognitive Therapy and Research, 36, 427–440.
- Hofmann, S. G., Sawyer, A. T., Witt, A., & Oh, D. (2010). The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. Journal of Consulting and Clinical Psychology, 78, 169–183
- Kabat-Zinn J. (2003). Mindfulness-based interventions in context: Past, present, and future. Clinical Psychology: Science and Practice, 10, 144–156.
- Kabat-Zinn, J. (1982). An outpatient program in behavioral medicine for chronic pain patients\\nbased on the practice of mindfulness meditation: Theoretical considerations and preliminary results. General Hospital Psychiatry, 4, 33–47.
- Kessler, R. C., Berglund, P., Demler, O., Jin, R., Merikangas, K. R., & Walters, E. E. (2005). Lifetime prevalence and age of onset distribution of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62, 593–602.
- Leichsenring, F., & Rabung, S. (2008). Effectiveness of long-term psychodynamic psychotherapy: A meta-analysis. Journal of the American Medical Association, 300,1551–1565.
- Linehan, M. M., Amstrong, H.-E., Suarez, A., Allmon, D., & Heard, H. L. (1991). Cognitive-behavioral treatment of chronically suicidal borderline patients. Archives of General Psychiatry, 48, 1060–1064.
- Nasser, M. (1987). Psychiatry in ancient Egypt. Bulletin of the Royal College of Psychiatrists, 11, 420-422.
- Norcross, J. C. & Goldfried, M. R. (2005). Handbook of Psychotherapy Integration. New York, NY: Oxford University Press.
- Rogers, C. (1951). Client-Centered Therapy. Cambridge, MA: Riverside Press.
- Segal, Z. V., Williams, J. M. G., & Teasdale, J. D. (2002). Mindfulness-Based Cognitive Therapy\\nfor Depression: A New Approach to Preventing Relapse. New York, NY: Guilford Press.
Authors
 Ingrid G. Farreras
Ingrid G. FarrerasIngrid G. Farreras is Associate Professor of Psychology at Hood College (Maryland). Her specialty area is the history of psychology and her research has focused on the establishment of the NIMH, the professionalization of clinical psychology, and how eugenics, Progressivism, and intelligence testing have shaped involuntary commitment laws for feeble-minded individuals.
 Hannah Boettcher
Hannah BoettcherHannah Boettcher is a doctoral student in the Psychotherapy and Emotion Research Laboratory at Boston University. She is a member of the Phi Beta Kappa Society and graduated with honors from Brown University. Her research focuses on understanding and treating anxiety disorders, with an emphasis on social anxiety and treatment outcomes.
 Stefan G. Hofmann
Stefan G. HofmannStefan G. Hofmann, Ph.D. is Professor of Psychology at the Department of Psychology at Boston University, see www.bostonanxiety.org. He is the 2013-2014 president of ABCT, the 2014 president of the IACP, the editor-in-chief of Cognitive Therapy and Research, and the Associate Editor of Journal of Consulting and Clinical Psychology.
 Q. Jade Wu
Q. Jade WuQ. Jade Wu is a doctoral student in the Department of Psychology at Boston University. She is a member of the Association for Behavioral and Cognitive Therapies, and the recipient of several prestigious awards, including the Boston University Dean’s Fellowship and the Clara Mayo Research Award.
Creative Commons License



 Therapeutic Orientations by Hannah Boettcher, Stefan G. Hofmann, and Q. Jade Wu is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. Permissions beyond the scope of this license may be available in our Licensing Agreement.
Therapeutic Orientations by Hannah Boettcher, Stefan G. Hofmann, and Q. Jade Wu is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. Permissions beyond the scope of this license may be available in our Licensing Agreement.
Creative Commons License



 History of Mental Illness by Ingrid G. Farreras is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. Permissions beyond the scope of this license may be available in our Licensing Agreement.
History of Mental Illness by Ingrid G. Farreras is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. Permissions beyond the scope of this license may be available in our Licensing Agreement.


