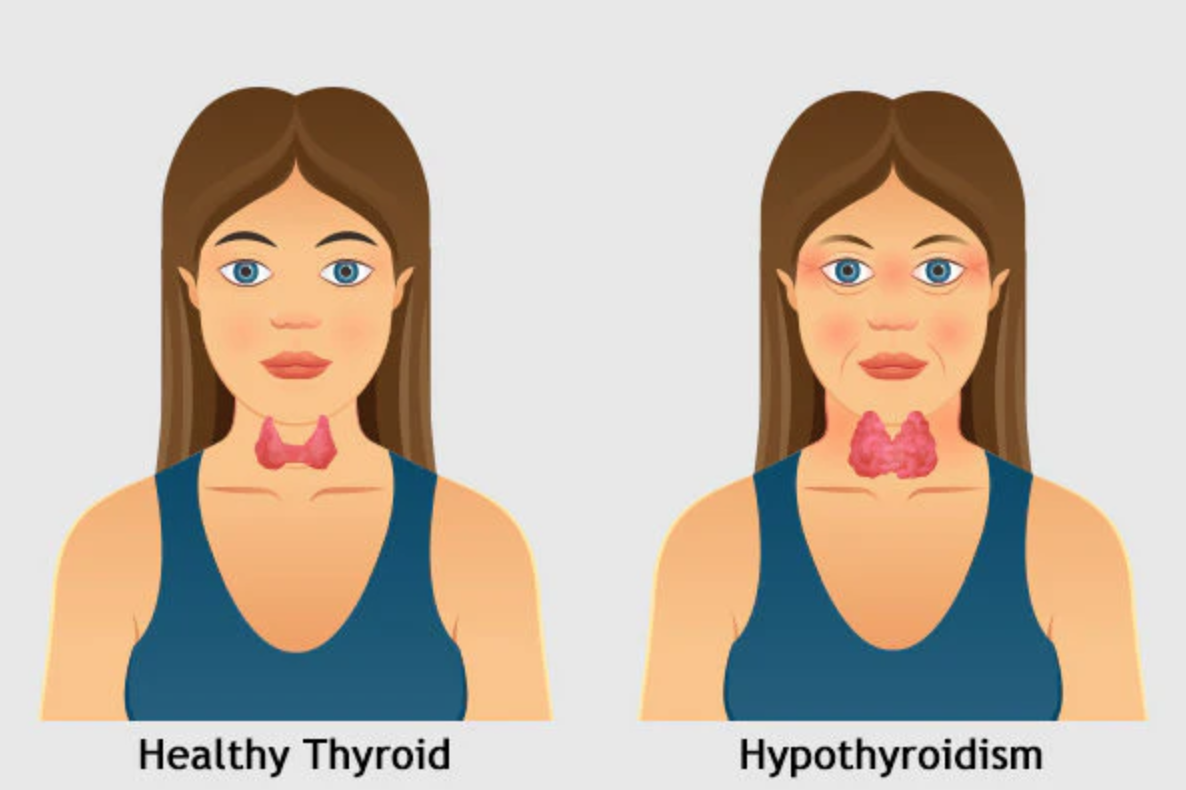
Patient A is a 59 year old female of Asian descent living with Hypothyroidism and GERD, well-controlled. The measured BP is 98/64 pulse 68, corresponding to normal. ASA 2.
Oral Interview
Medications
- Hypothyroidism: Synthroid (levothyroxine) 50mcg taken for 10 years. There are no notable side effects on dental treatment.
- GERD: Nexium (esomeprazole magnesium) 40mg taken for 1.5 years. There are no notable side effects on dental treatment.
Dental considerations: xerostomia, halitosis.
At-Home Care
- Powered toothbrush, two times per day.
- Sensodyne dentifrice, two times per day.
- Sensodyne is composed of sodium fluoride and potassium nitrate, which helps chemically desensitize nerve fibers and reduce tooth sensitivity.
- Floss pick, one time per day.
- Water floss, three times per day.
- Listerine mouthrinse, one time per day.
- Metal tongue scraper, periodically.
Assessments
Extra-/Intra- Oral Examinations
- Prominent observation: the left of the thyroid is slightly elevated. Patient reports no pain.
- Gingiva presents with generalized pale-pink, stippled, firm and blunted papillae. Gingival margins apical to CEJ. Localized red, smooth blunted papillae on maxillary posterior lingual surfaces with mild bleeding upon probing.
Dental Charting
- Localized occlusal amalgam and Class V composite restorations on posteriors.
- Suspicious carious lesions on occlusal surfaces on third molars.
- Due to the suspicious lesions, the patient is at high caries risk. A referral is given for further comprehensive evaluation and restorative work.
- Since GERD was noted, dental erosion was assumed however, none was clinically detected.Periodontal Charting
- Generalized 2-4mm PD with localized 5-6mm PD on posteriors.
Vertical Bitewings – Radiographic Statement
- Calculus: generalized on posteriors. Crest of bone: generalized 3-4mm apical to CEJ, 45% horizontal bone loss. Suspicious carious lesions: none detected radiographically.
Periodontal Status
According to the assessments and radiographs, the patient has generalized Periodontitis Stage II, Grade B with heavy interproximal calculus and mild staining.
Treatment Plan & Implementation
Based on the initial oral interview, the patient’s oral home care is deemed adequate. The goal is to improve her current techniques in brushing and using an interdental aid. On the initial visit, the Modified Bass brushing method is implemented on a typodont for educational purposes. Then, the patient utilizes her toothbrush on her teeth to repeat the motion of angling the toothbrush at 45 degrees at the gingival sulcus with light pressure. On the second visit, proper use of a floss tape is implemented. Although she uses interdental aids of a floss pick and water flosser, the heavy calculus clinically seen does not reflect her efforts. Teaching the correct ‘C’ technique of floss tape allows the patient to better target the plaque and bacteria at the sulcus. In turn, the risks for further potential caries, bone loss, and halitosis are decreased. The patient is advised to incorporate frequent water intake to reduce symptoms of xerostomia. She may visit her general dentist to get prescribed a mouthrinse, Biotene, to help stimulate saliva concentration in the oral cavity. Increasing fluid in the oral cavity will lower the proliferation of acid-producing bacteria, like Streptococcus mutans, that cause caries.
Initial Visit: Expose 4VBWs with written patient consent, educate oral hygiene instructions (OHI), scale quadrant 1 to completion with Ultrasonic and hand scalers with prior application of topical anesthetics: 20% Benzocaine and Oraquix: 2.5% lidocaine + 2.5% prilocaine for sensitivity.
Second Visit: Educate oral hygiene instructions (OHI), Scale quadrants 2, 3, 4 to completion with Ultrasonic and hand scalers with prior application of topical anesthetic: 20% Benzocaine and Oraquix: 2.5% lidocaine + 2.5% prilocaine for sensitivity. Finish treatment with engine polishing with prophy paste and 5% NaF varnish.
Evalution
In the second visit, the gingiva of the previously scaled quadrant 1 was re-evaluated. Patient also reports implementing the Modified Bass brushing technique into daily routine. The lingual surfaces of the maxillary posteriors were noticeably less inflamed and red with no bleeding upon probing. The results are evident of both the clinician’s and patient’s efforts in effectively removing plaque.
Based on the assessments and evaluation, it is recommended for the patient to return every 3-months for periodontal maintenance.



