Case 1: Heavy/type II perio/Never had a cleaning
38 yr old Hispanic male with a very compromised medical history. Pt was suffering from anxiety, depression and PTSD since he was 16 years old. He had sleeping problems snd was taking for it. Pt also suffered frequent nosebleeds. He reported he had never had a cleaning and did not floss or rinse. He only brushed using horizontal strokes and a hard bristled toothbrush. As a result of his negligent attitude, he had several active carious lesions and decayed teeth including #8M, 9M, 12MOD, 19MOD, 31MOD. He also had ledges of calculus as a result of inadequate home care and never visiting the dentist.
V1: At first meeting, pt’s medical history and vitals were taken, and medications looked up. All assessments were completed. Perio charting showed several 5-6 mm pockets in both anterior and posterior teeth. Because there were ledges of calculus in between his teeth, those were not even true readings. Because of deteriorating perio condition and several active caries, digital FMS radiographs were taken. The xrays confirmed caries in #8, 9, 12, 19 and 31. Pt was encouraged to use the modified bass method of brushing because his accretions were mostly on the cervical 1/3 of the teeth. I also encouraged him to brush twice a day, especially at night, so plaque doesn’t build overnight. He was also refered to a list of hospitals within his neighborhood so he could get his caries taken care of.
V2: Prior to his second appt, pt reported he was very apprehensive about the cleaning. Considering his mental condition and anxiety, I assured him over the phone he would be fine, we had several hygienists and dentists on the floor and that we would use local anesthesia on him for sensitivity. Pt however did not want to be anesthesized (was scared of needles), so we ended up using Oraqix to scale the UL and LL quadrants. Pt took the treatment well and reported his gums felt much better once the calculus ledges were removed. He said he could even feel the difference with his tongue. I noticed he had higher amount of calculus on the right side than the left (he was right handed, so brushed the opposite side better). Keeping this mind, I reiterated the bass method to him encouraging him to pay more attention to his linguals and the right side of his mouth.
V3 Because pt’s right side had heavier and nore tenacious calculus, I divided scaling the right side into 2 visits. Rather than Oraqix, I anesthesized pt using 2% lidocaine w/ 1/100,000, buccal and mental infiltration. Then I scaled the LR quadrant using the cavitron and hand instruments. Pt reported less sensitivity than previously and was thankful that he coukd finally feel his gingiva. With the deposits mostly removed, it was time to teach him flossing. I showed him how to use floss picks to clean in between teeth as this would be easier for someone starting out.
V4: In the last visit, pt reported he felt much less anxious about going to the dentist and akready made an appt for endodontic and restorative work on his decayed teeth. This time he felt comfortable being scaled with just Oraqix. So I scaled his UR quadrant with Oraqix, hand instruments and the cavitron. I also did necessary rescales and engine polished the pt using fine polish to remove leftover biofilm and stains. I applied 1.1 % NaF varnish since pt was already at high risk for caries. Pt promised he would keep his 3 month recare appt and thanked me for helping him cure his dental anxiety and giving him a new smile.



Case 2 Medium/Type II perio with type III localized/Arestin case
Pt was a revisit pt from clinic. She was 74 yr old Caucasian female, non smoker but social drinker. She was suffering from Hoshimatos disease (a form of hyperthyroidism) and type 1 diabetes. Her meds included Humalog and Synthroid. Care had to be taken so her blood sugar was not too low prior to dental appts. Pt had several 6-7 mm deep pockets in the molar region and generalized horizontal bone loss. Due to limited manual dexterity, pt was always getting food lodged in her back pockets. She also had an extremely limited opening (she could only open 2-3 mm) which made scaling extremely difficult. Pt’s gingiva was pink without stippling, soft, bulbous in the mandible, some missing and cratered papilla and there was moderate bleeding upon probing.
V1: Prior to the visit, I called the ot to ensure she had eaten and taken her diabetic medication to prevent hypoglycemia. All assessments were conducted, including a thorough perio chart listing areas of recession, pocket depths and BOP sites. Pt was taught the use of a reach floss holder to clean the gunk out from her pockets. Considering her limited opening, this was a better option than floss piks or regular floss. Pt bought two floss holders from clinic for home use. A biteblock was used horizontally to keep the pt’s mouth open because she could not support it on her own. The UR quadrant was scaled using Oraqix. Pt took treatment well and said she would try the floss holder at home.
V2: Pt reported she was still having difficulty accessing the back teeth and could “feel” food lodged back there. I recommended she start using different brushhead fir her electric toothbrush. I even showed her some from clinic and she bought the replaceable heads as well as the new brand of toothbrush. Pt’s LL, UL and LR quadrants were scaled, again using the bite block. Even with the bite block, the pt could not open large enough to fit the cavitron hand piece in her mouth. So I had to use complete hand instrumentation, directed by indirection vision to scale her calculus (which was mostly on the lingual mandibular teeth). I used all horizontal strokes with my hand instruments because her restricted opening did not allow me room to scale up cervically. Pt’s teeth were polished using fine paste on natural teeth, making sure to leave her porcelain crowns and amalgam fillings out of the equation.
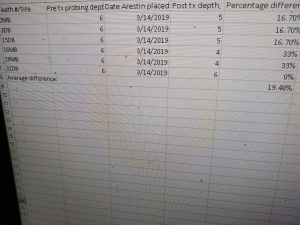
V3: Pt was chosen for arestin placement on 6 sites because she had deep pocketing that did not go down with scaling. A PAN radiograph was exposed prior to arestin placement. It confirmed generalized horizontal bone loss not to mention a periodontal abcess on #5. Pt was given an adult referral for the abcess. Pt was also explained that arestin is an antibiotic that will help reduce gingival bleeding, inflammation and pocket depths. The 6 sites chosen for the arestin placement all measured 6mm and were located on : . After placing arestin, pt was instructed not to chew hard sticky foods or floss in those areas for a week.
V4: Pt reported for revaluation for arestin. All of the sites (except for 1) decreased to 4-5 mm. The pt also reported less pain when probing in those sites. The gingiva in the selected areas also showed less sponginess and inflammation with no more bleeding upon probing. Pt was encouraged to keep up with homecare and report back in 4 months for her recare appt.

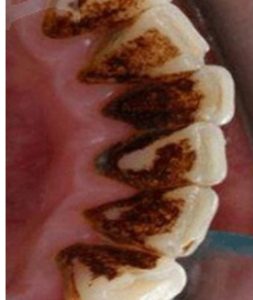
Case 3 Heavy/perio type III/Chain smoker with heavy black staining
41 yr old Indian male who had been smoking 30 cigarettes a day. He had few systemic conditions including hypertension, diabetes type 2, and hepatitis. His meds included . His last cleaning was more than 5 years ago. He had generalized hard black staining on all of his teeth due to accumulation of tobacco residue. He was also suffering from periodontitis due to poor oral care and lack of oral hygiene. His pocket depths were 6-8mm in posterior teeth and 4-6mm in anterior teeth.
V1: After med history and perio charting, it was decided pt was suffering from deep pocketing, recession and periodontal disease. His gingiva was pink without stippling, mostly fibrotic tough consistency, with blunted papilla, slight bleeding upon probing. He also presented with intraoral findings, including bilateral leukoplakia, clustered red lesions on the hard palate and extremely yellow coated tongue. Pt reported he did not brush his tongue and was suffering from halitosis, due to heavy smoking. Pt was taught how to use large plastic tongue scraper to clean his tongue daily. An FMS was exposed which revealed generalized horizontal bone loss and vertical bone loss in the mandibular molars . Pt was also warned that heavy smoking increases the chance of oral cancer by 10 fold and given suggestions on how to quit smoking. He was also given a referral to a pathologist for leukoplakia. Finally the UR quadrant was scaled using mostly the cavitron to remove the extremely heavy smoker stains. Then hand instruments were used subgingivally to remove remaining calculus.
V2: Pt reported he did not floss, so he was taught C shaped flossing to clean in between teeth. Since it was extremely difficult to remove his heavy stains with just the cavitron, I used the engine polishing unit to remove as much of the extrinsic staining as possible prior to scaling. The coarse paste engine polish was more efficient than water cavitation at dislodging the black residue from tobacco smoke. Then I went in with my hand instruments to remove subgingival calculus in LL, LR, UL quadrants. Oraqix was used for pain management. Pt was given a mirror so he could see what a difference the cleaning had made. He was encouraged to stop smoking if he wanted to keep up the shiny appearance of his teeth after the cleaning. The patient surprised me by saying he has already started smoking less since the first visit because he did not want the tobacco residue to rebuild. He did not have insurance and could not afford regular cleanings. So he would try to maintain the cleaning by smoke less. This is the most monumental change I made in a patient’s mentality and mindset regarding his mental health and I was proud!


Case 4: Heavy/type II perio/autism/inadequate oral care
Pt was 22 yr old Indian male with self limiting conditions of autism and ADHD. He had problems listening, paying attention and remaining still in the dental chair. He had inadequate oral care at home. He did not floss at all and had limited manual dexterity when it came to brushing. He only brushed the posterior teeth with a manual brush using the Fones method. He did not like brushing the front teeth as he was very sensitive there. As a result, he had both sub and supra deposits in the anterior teeth and interproximal deposits in the posterior. He had no caries but had moderate gingivitis with some 5-6 mm pockets due to inadequate self care. BWS from 6 months ago showed he had some localized vertical bone loss in the molar region due to accretion buildup. His habits needed to be changed.
V1. All assessments were completed. Gingiva appeared bright red, erythamatous, soft spongy consistency, spontaneous bleeding upon probing. Because of his mental condition, pt did not want to be “poked” with a probe. He had to very carefully be shown with a typodont that we were going in the sulcus (the space between the teeth and the gums) to measure pocket depths and that he would not get hurt. Seeing his interproximal deposits, I inquired what kind of oral care he used at home and he responded he did not floss at all. I used this opportunity to disclose his mouth and show him the interproximal biofilm he had accumulated due to not flossing. He was very surprised to learn how much of his mouth was covered in red. I then showed him how to use floss piks to clean in between teeth and cleaning the piks with gauze and Listerine in between. I then scaled the UL quadrant using Oraqix, hand instruments and cavitron. For his deeper pockets in the back, I used the subzero instruments so the longer shank could allow deeper scaling.
V2: Pt reported he had not started using the floss piks as he wasn’t really interested in his oral health. His gingiva still appeared erythamatous, soft and spongy, though with less bleeding upon probing than last visit. Pt was also not brushing his teeth properly. So for this visit I decided to teach him to use an electric toothbrush aimed at 45 degrees towards the Gingival margin to clean out cervical sub and supra accretions. He said he did not like the sensations of the bristles on his gums. I then showed him how to turn down the vibrations to low and sing a somg while brushing to distract him enough to complete a 2 min cycle. I then scaled his LR and LL quadrants using Oraqix and hand instruments. Because he did not like loud sounds and vibrations, I decided not to use the suction or the cavitron to scale. The pt also was very fidgety in the chair, so I showed him how all the patients, including the one right across from him were very excited to get the cleaning so he should be too. This seemed to calm him down. I also covered him with his jacket and played his favorite music on my phone so he would feel more comfortable while in my chair.
V3: Pt’s gingiva began to show a noticeable improvement, appearing less spongy and erythamatous, more contoured and regular margins, pinker, firmer, with less BOP. He was no longer feeling as sensitive in the front teeth when I touched him there. This was a good time to reiterate to him to start flossing. This time I bought mint flavored floss piks for him to floss with. He liked the minty flavor and said he will try to floss more. This was a start and I did not push him to do it daily. I scaled the UR quadrant of the pt using Oraqix and hand instruments. This time the pt was less fidgety and took the treatment well. He had learned that a little bit of pain and sensitivity in the dental chair now can prevent him from developing more serious health issues such as periodontitis later. After scaling, I polished the pt’s mouth with minty fine paste to remove the extrinsic staining. He was given fluoride varnish to prevent against cavities and a 4 month recall. Pt appeared more interested in his oral health and he will return for cleaning. I am glad I was able to condition him into being a better dental patient and he did return the following semester to get a cleaning done by me.


Other cases I have worked on
786 Case Presentation on hypertensive/diabetic patient from third semester


