Case Study #1 – Arestin Treatment (October 13, 2017)
Assessments: 44-year old female. Light case value/Type II periodontitis. Patient is overall in good health with a blood pressure of 123/89 and pulse of 85. ASA II. Vital signs were within normal limits and being controlled by taking medication for high blood pressure. This patient presents with hypertension and takes Norvasc (Amlodipine) 10mg 1x a day for this systemic condition. An adverse reaction of this drug includes gingival hyperplasia with may modify the oral cavity.
After conducting a thorough intraoral and extra oral exam, I found a 2mm raised light pink lesion with regular borders on the labial mucosa, opposite tooth #21. The faculty and I concluded that this was a possible fibroma and no referrals were required. Patient has attrition present on #6-#11 and #22-#27 and also localized diastemas were documented. Localized amalgam restorations on the maxillary posteriors were present and all in tact. No tooth anomalies and no caries.
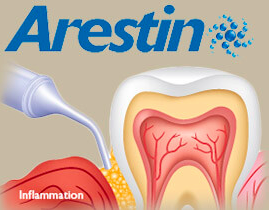
Periodontal exam: Gingiva is localized moderately inflamed in the posterior regions. The gingiva is also dark pink and pigmented, spongy and bulbous. Patient is classified as type II periodontitis due to 3-8mm probing depths and localized moderate bleeding upon probing. No clinical attachment loss. Based upon the assessment, yes this patient was approved for Arestin. After completing periodontal assessments, I concluded that this patient would be a great candidate for Arestin treatment. The sites that were chosen for Arestin were: #14-DB (8mm), #14-DL (6mm), #14-ML (5mm), #15-MD (7mm), #15-DB(7mm), #15-DL (5mm), #15-ML (5mm), and #18-ML (5mm). This patient did not qualify for new radiographs due to the bitewings present that were taken at our clinic is 2015.
Oral hygiene: This patient was a light case value due to the very light areas of calculus found on the mandibular anteriors Plaque score: 0.8. I interviewed this patient about her oral hygiene and documented that she flosses once a day and brushes twice daily. This patient seemed very meticulous about her oral hygiene!
- Visit 1: completion of all assessments, OHI plaque score and teaching a modified bass method, full mouth scaling, polishing and applying a 2% neutral sodium fluoride treatment.
- Visit 2: Reviewed medical history, evaluated the areas approved for Arestin treatment, documented the probing depths, placed Arestin in those areas, and gave the patient post-op instructions.
- Visit 3: evaluated the areas that I have previously placed Arestin and documenting the new probing depths.
- Based on my analysis and interpretation of the data gathered during the assessment, I applied a 2% neutral sodium fluoride treatment for not only prevention of caries, but also upon the patient’s request. I also recommended a chemotherapeutic mouth rinse due to this patient’s periodontal pockets. No medical, social or psychological factors impacted the treatment of this patient.
Arestin Evaluation visit: (November 10, 2017)
4 weeks later, I was able to evaluate the treatment of Arestin on my patient. I lightly probed each area and documented the results. The patient and I were amazed that most of the pockets decreased! The following probing depths were recorded: #14-DB (4mm), #14-DL (4mm), #14-ML (3mm), #15-MD (3mm), #15-DB (4mm), #15-DL (5mm) this was the one probing depth that remained the same, #15-ML (4mm), and #18-ML (3mm). Having the chance to place Arestin on a patient in need of a treatment like this was such a rewarding experience!
Case study #2 (Management of a patient with a systemic disease)
Patient presented to the clinic for a dental cleaning with the concern of not being seen in over 3 years due to “previous extractions.” After reviewing medical history, the information was found as follows:
- Patient is allergic to latex and sulfa drugs and if contact was made, patient would develop a puffy throat, itching and rash.
- Patient was diagnosed with heart disease one year ago after having a heart attack. No premedication was required for this visit as per physician.
- Patient currently takes Atorvastatin 1x a day, Clopidogrel 1x a day and Metroprolol 1x a day to manage this systemic condition. Classified as ASA II.
Assessments: 55 year old Caucasian male. Blood Pressure: 128/85, pulse: 73. EO/IO exam: slight crepitation of TMJ during lateral deviation and scalloped tongue. Checked macule on commissure lip pit from previous visits documented in computer. Patient stated that he plans to get it removed. Dental: Class I occlusion bilateral, overjet: 3mm, overbite: 30%. Localized amalgam and composite fillings present. Peg laterals #7 and #11 and generalized attrition. Patient stated that he grinds his teeth at night but cannot use a mouthguard due to difficulty breathing at times. Periodontal: 3-4mm probing depths and localized mild recession. Gingiva is dark pink, firm, stippled with generalized inflammation. After exploring for calculus, generalized subgingival and supragingival calculus deposits were found along with staining on the mandibular lingual anteriors. Patient is a heavy case value/type II periodontitis.
Treatment: After an oral hygiene interview, patient revealed that he uses an electronic toothbrush at home and uses Sensodyne toothpaste for sensitivity to cold. I demonstrated the proper angles of the power brush and discussed that he should be brushing for 2 minutes 2x a day. I scaled all 4 quadrants with the ultraosnic and hand instruments, polished with medium paste, and gave a 5% fluoride varnish treatment with post-op instructions. I instructed the patient to come for his next visit in 3 months.
Reflection: After treating a patient with this systemic condition, I realized how important it is to go through an extensive medical history with a patient before beginning treatment on them. Sometimes you have to continue asking questions to the patient until they release all the information they have. After asking many questions about medications and why he has not been seen in over 3 years, I finally got the patient to tell me that he had a heart attack only a year ago. Sometimes patients do not realize that their dental hygienist needs to know information regarding any kind of condition a patient may have. It is my job to explain why it is so important and that we need to make sure our patients are safe undergoing dental treatment.