My patient Mr. A is a 52 years old Russian male. His vitals were 110/78 with a pulse of 75. He is a ASA I patient as he is a non-smoker and drinks alcohol occasionally, 1~2 glasses every week. His last dental visit was for a check up on a mandibular anterior fracture on 04/17/2019.
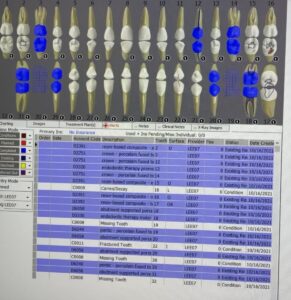
There were no findings on the extraoral examination but his dry lips. A coated tongue, bilateral mandibular tori, and bilateral linea alba were found during intraoral examination. His occlusion was bilaterally class I with 3mm of overjet and 90% of overbite. He also had localized attrition on maxillary/mandibular anteriors. According to his dental charting, #6 was rotated towards lingual, #32 was not clinically present, and two mandibular bridges were also present; #18 to #20 and #29 to #31.
His gingiva was pale pink, stippled, generalized red GM, puffy; bulbous/soft and spongy papilla. He had generalized moderate marginal gingival inflammation, and generalized BOP with generalized 4-6 mm depth on posteriors. Generalized mandibular anterior supra/subgingival calculus, localized subgingival calculus on maxilla anterior were explored.
When I explored around the bridges, there was tenacious calculus everywhere under the bridge.
For his treatment plan, FMS, full mouth scaling, engine polish, application of 5% sodium fluoride varnish were planned and it was discussed with the patient.
FMS at 70 kVp and 7 mA was exposed during his initial visit. Radiographs revealed that #32 is not present, and root canals were done on #12 and #18. Mandibular bridges, #18 to #20 and #29 to #31, were exposed with localized 10% radiographic bone loss on mandibular posteriors. Also, there was generalized subgingival radiographic calculus on mandibular posterior and anteriors without decay.
His plaque index score came out as 1.5; fair. The biofilms were mostly present on cervical third and interproximally. Demonstration of super-floss for his bridges was conducted for the patient education, and he was able to perform the correct technique.
Patient was successfully treated with full mouth scaling using ultrasonics and hand scalers, engine polished, and application of 5% sodium fluoride varnish was provided.
It was a challenging case for me, as he was my first patient with bridges containing heavy subgingival calculus. After his full mouth scaling, Mr. A was very appreciative and satisfied with the hard work that was done and the new freshness of his oral cavity.