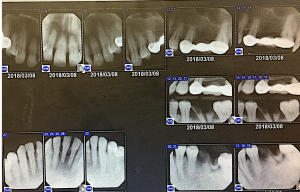
Clinical Case I – Treatment of Patient with Stage I Hypertension
Patient M.F., is a 47-year-old Middle Eastern female who presented with Type II Periodontitis and heavy supragingival and subgingival deposits. This patient was taking Losartan 50 mg once daily for control of her hypertension. Her vital signs were within normal limits during treatment. Extra-oral examination revealed no significant findings. Intraoral assessment indicated signs of neglect as a result of dental anxiety. The patient had retained root tips on teeth #18 and #19 and tooth #2 was possibly non-vital with a parulis on the hard palate. The lesion presented as red, raised and 2.5 mm in diameter. Mobility was present on teeth #23-26. The patient’s gingiva presented with melanin pigmentation, generalized moderate inflammation and localized areas of spongy tissue. There were generalized 2-3 mm PD’s with localized 4-6 mm PD’s and moderate BOP. As a patient with high blood pressure, I was mindful that she may experience orthostatic hypotension as she is raised from a reclined position. To make the patient more comfortable and reduce her anxiety, I raised the dental chair slowly and let her sit for some time before getting up. She was also advised to always take her medication and have a meal prior to treatment. The patient was scheduled for multiple appointments so that she would not be overwhelmed and to reduce her anxiety. In order to assess for bone loss, I recommended the patient have a FMS of radiographs taken. One of the biggest challenges I faced during this clinical case, was the patient’s severe gauge reflex. However, I was able to successfully complete 20 diagnostic radiographs which were critical for a full assessment. Upon evaluation of the radiographs, localized horizontal and vertical bone loss were indicated and possible carious lesions. The patient was given a referral for treatment of caries, retained root tips on #18 and #19, extruded tooth #1 and likely non-vital #2.

 _______________________________________________________________________________________________________________________
_______________________________________________________________________________________________________________________
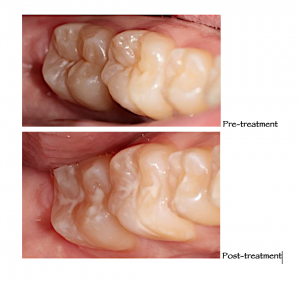
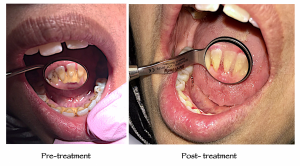
Clinical Case II – Sealant Placement
Patient A.G. 21-year-old Caucasian male, ASA I. He presented with Type I Gingivitis and generalized medium deposits. The patient had no clinical or radiographic evidence of active caries present on teeth #30 and #31. Due to poor OHI, high intake of sugar, acidic food products and past dental caries, I recommended he have sealants placed on #30 and #31 to prevent future dental decay. The sealants were placed with the use of a rubber dam.
_______________________________________________________________________________________________________________________
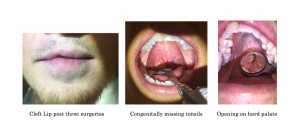
Clinical Case III – Cleft Palate
B.C., 35-year-old Caucasian, male, ASA I. No medication or known allergies. The patient reported with a cleft lip and cleft palate that had been surgically repaired. He reported undergoing three surgeries to treat the condition. However, after surgery, his dentist recommended he have a palatal expander placed before undergoing orthodontic treatment. As a result, this caused the cleft palate he once had sealed to open again. Upon intraoral examination, I noticed the patient did not have any tonsils and he also had an unusually smaller uvula. The patient reported his tonsils were congenitally missing. He had crowding on the mandibular anterior teeth and tooth #7 was also congenitally missing. Since the patient was an avid green tea drinker, he had generalized black line staining. Although he would have been a perfect candidate for air polishing, I decided it was contraindicated for him due to the cleft palate opening which lead right into his sinus cavities. The powder from the air polishing would have easily entered into his sinuses and could have caused a potential bacterial infection. Instead, to complete treatment I used the cavitron, hand instruments and hyrdorgen peroxide to loosen the stains. I finished by performing a rubber cup polish using coarse paste. During treatment, I also made sure to use a slightly wet gauze to block off the opening on the palate so to avoid any particles or debris from entering.
 _______________________________________________________________________________________________________________________
_______________________________________________________________________________________________________________________
Additional Clinical Case findings:
I.G., 56 year old caucasian female, ASA I. Presented for a prophylaxis and radiographs. A panoramic radiograph was taken and upon assessment I noted an unerupted supernumerary tooth adjacent to #24 and #25. The patient was given a referral to their dentist for evaluation and advised to have it monitored. A copy of her radiographs were also given to her.
_______________________________________________________________________________________________________________________
S.P., 19 year old middle eastern male, presented for a scaling. Upon assessments his third molars were not clinically present. A panoramic radiograph was taken and upon review, I noted a radiolucency with a radiopaque border on the posterior 1/3 of the ramus on the mandible. Although professors thought it was a foreign object in the patients mouth or a piercing of some sort, I persisted that it was a Stafne Bone Cyst due to its signature radiographic appearance and location. The oral pathologist and dentist evaluated the patient’s radiograph and confirmed my findings. Although there is no treatment necessary for it and it is not a true cyst in nature, the patient was advised to follow up with his general dentist every six months.

_______________________________________________________________________________________________________________________
S.S. 21 year old hispanic female, presented with no clinically present maxillary third molar #16. A panoramic radiograph was taken which confirmed the patient had a supernumerary third molar adjacent to tooth #1 and also multiple third molars superior to impacted third molar tooth #16. The patient was given a referral for evaluation by an Oral Surgeon.