This clinical case study was based on a patient that I treated in clinic who exhibited signs of dental anxiety. Dental anxiety and phobia can result in avoidance of dental care. It is a frequently encountered problem in dental offices. The initial interaction between the dental hygienist and the patient can reveal the presence of anxiety, fear, and phobia. In my clinical experience, I have found that behavior modification therapies such as the use of relaxation breathing, positive reinforcement, stop-signaling, and “tell-show-do” modeling are very effective in reducing levels of dental anxiety and fear.
DEMOGRAPHICS
Name: C.K.
Age: 30 years old
Case/Type: Medium/Type I
ASSESSMENT
This patient was a healthy individual, ASA Type I, who had no allergies, no recent surgeries or hospitalizations and she did not drink alcohol.
C.K.’s blood pressure was 118/81 and her pulse was 71 beats per minute.
C.K. was a non-smoker.
C.K. did not require any premedication for dental treatment.
C.K. did not have any systemic conditions.
C.K. takes a daily multivitamin and Loestrin for birth control (1 tablet per day).
Loestrin is a contraceptive pill that women take to prevent getting pregnant. It is an estrogen and progestin combination drug which has female hormones that prevent ovulation (the release of an egg from an ovary).
ORAL PATHOLOGY (Extraoral and Intraoral findings)
C.K.’s extraoral exam had no significant findings. A maxillary torus palatinus and bilateral linea alba were found during her intraoral exam.
DENTITION
C.K.’s class of occlusion was Class I with 80% overbite and 2 mm overjet.
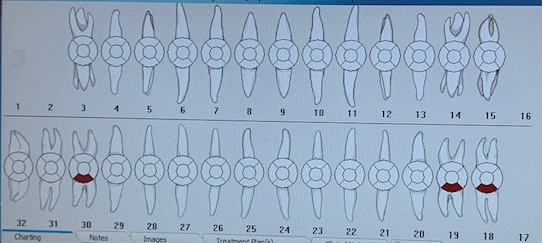
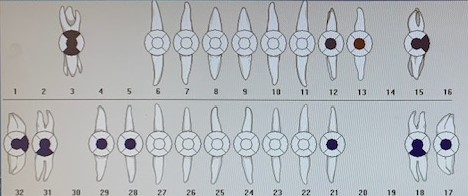
This patient had generalized mild fluorosis on both anterior and posterior maxillary and mandibular teeth. She also exhibited generalized attrition on teeth #s 6-11 and 22-27. C.K. had crowns on teeth #s 19 and 30, an occlusal composite restoration on teeth #s 32, 2 and 4, a distal composite restoration on tooth # 12 and a distocclusal composite restoration on tooth #14. She was missing teeth #s 1, 15, 16 and 26. Teeth #s 1, 15 and 16 had been extracted and tooth #26 never erupted.
C.K. had four occlusal cavities present on teeth #s 31, 20, 18 and 17.
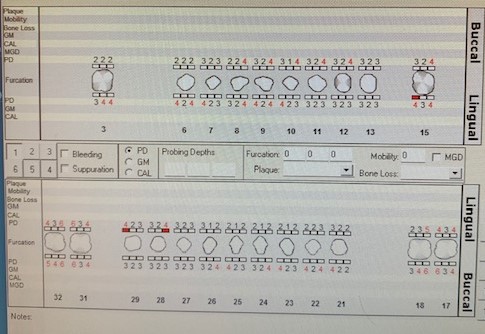
PERIODONTAL
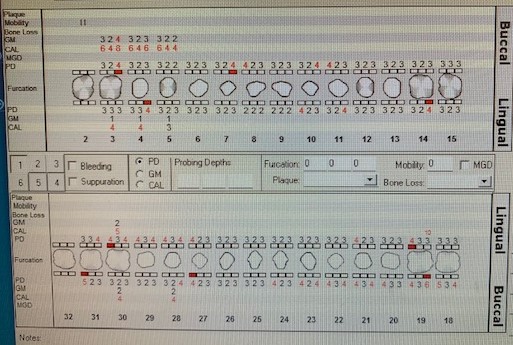
C.K. was classified as a Medium Case, Type I. This patient’s probing depths were between 1-5 mm. She had generalized bleeding upon probing and recession on teeth #s 30, 28, 25, 24, 5, 6 and 10.
The gingiva of the anterior mandible was red with rolled margins and the anterior maxilla was pink and firm with a line of red on the lingual cervical third of tooth #30. There were red margins on the right of the lingual maxilla.
ORAL HYGIENE
C.K.’s initial plaque score was 2 (poor). At the time of her subsequent appointment, the plaque index score was 0.8353 (fair).
C.K. had generalized subgingival calculus present on the mandible and localized on the maxilla, on teeth #s 2-4 and 10-14.
Based on the patient’s current oral homecare practices, I made several recommendations for modification. C.K. had more plaque present on the anterior facial teeth than the posterior buccal and lingual. C.K. was using a manual, medium bristle toothbrush and was flossing once per day with floss gliders. She stated that she uses original Listerine once per day. She also uses the back of her toothbrush to clean her tongue and she had no oral piercings. I recommended that C.K. use a soft-bristle toothbrush and demonstrated the Modified Bass tooth brushing method, so that she could learn how to concentrate on cleaning at the gum line and to focus on the anterior areas. I showed the patient how much plaque was accumulating interproximally as well as at the gum line. I also recommended that she switch from Listerine to Act, since that contains fluoride and she had four active caries.
At the patient’s next visit, I demonstrated flossing with waxed dental floss and the patient practiced the technique.
RADIOGRAPHS
C.K did not require bitewing radiographs.
TREATMENT MANAGEMENT
On the first visit, C.K. filled out the medical history form and we discussed her current oral home care regimen. I conducted an intraoral/extraoral examination, charted her entire dentition and completed her periodontal chart (probed her entire dentition). Then, I assessed her level of calculus. I determined the treatment plan for this patient which consisted of two more visits. I also gave C.K. a referral letter to a dentist to have the suspicious carious lesions further evaluated as well as an ill-fitting crown.
On the second visit, I reviewed C.K.’s medical history and it was determined that there were no changes. The patient was not taking any new prescription or OTC medications. I took C.K.’s initial plaque score and I recommended revisions to her current oral homecare regimen. I used topical anesthetic because the patient experienced mild sensitivity and scaled the entire dentition. After scaling was completed, it was determined that there was residual calculus on teeth #s 2, 3, 8, 10, 12, 13, 22-27, 29 and 31.
During the third visit, I reviewed C.K.’s medical history and it was determined that there were no changes and she was not taking any new medications since the previous visit. I then proceeded to take the patient’s subsequent plaque score, which showed an improvement since the initial evaluation. I demonstrated flossing to the patient and she practiced the technique. Her gingiva showed moderate improvement, with minimal bleeding upon exploring. I proceeded to rescale the areas with the residual calculus from the previous visit. I used topical anesthetic. After rescaling was completed, I used engine polishing on the full mouth with fine paste and applied neutral sodium fluoride varnish 0.5%. I advised the patient that she should return for a recall visit in three months.
C.K. had one medical factor that affected her treatment – she has a very small mouth. It was very difficult to reach her posterior teeth. To work around this, I would tell C.K. to relax her mouth a little bit so that the mirror could be used to retract the buccal mucosa more. When she opened wide, this tightened that area too much and it was too difficult to access.
One social and psychological factor that impacted the patient’s treatment was that she is my sister. I found this to be incredibly challenging, because I should have realized before having her as my patient, that she is very fearful of any medical treatment whatsoever. Initially, I thought that the fact that I am her sister would make her calmer and more trusting.
It was very difficult not to go back and forth between being dental hygiene student and sister. I found myself switching on and off between being professional and speaking to her as I would speak to any patient and then speaking to her like I do outside of clinic, as her sister. Every time I picked up an instrument, her eyes would widen, she would ask me what I was going to do with it, and she was very sensitive. It was even more frustrating because she did not want Oraqix, even after I thoroughly explained to her what it was. Additionally, she was very stressed during her third visit, even though this was the visit that had the least invasive procedures done out of the three. This was because she had an exam the next day and was trying to make it in time for tutoring. These factors – the small mouth, her nervousness, anxiety, fear and stress are all issues that I will face when treating various patients, but it’s somewhat harder when it’s a family member for some reason.
C.K. was recommended to use a soft bristled toothbrush and to use the Modified Bass toothbrushing method. I realized during her follow-up visit, that she was practicing the technique incorrectly. I retaught it to her but she found it difficult when she then practiced on herself. It was during this visit that I realized that a lot of the plaque buildup on her posterior teeth was because she had such a hard time maneuvering the toothbrush in that area. A regular, adult-sized toothbrush is way too big for her mouth. I advised the patient to use a child-sized toothbrush and/or an end-tuft brush, especially to reach the posterior regions of her mouth. The only regret I have regarding this is that I did not have a child-sized toothbrush available to give her at the time and to demonstrate with her during the visit. Regarding flossing, the patient also had some difficulty using the traditional waxed floss. She was a little frustrated, but I explained to her that all she had to do was practice and take her time.
C.K was referred to a dentist for further evaluation of the four suspicious carious lesions in her lower left and right quadrants.
In hindsight, I would have changed my treatment plan by extending the number of visits for this patient to four instead of three. Instead of scaling the entire dentition in one visit, I would have only scaled two quadrants and made the patient return for scaling of the remaining two. I would have done this because of the patient’s anxiety and fear of dental treatment. This would cause less trauma for the patient and would be a way for the patient to become accustomed to the treatment, the general dental clinic setting and the procedures to be performed. In general, I would also be able to spend more time explaining the procedures and easing the patient’s anxiety. Regarding patient education, I would have recommended that the patient use a child-sized toothbrush during the visit when I taught her tooth brushing. I felt responsible because she tried the technique that I showed her, but she had a lot of difficulty because she was still using the wrong sized toothbrush.
EVALUATION
The patient responded well to the interventions that were introduced and taught but I think that she has to spend some more time practicing the techniques.
I think that this patient was somewhat interested in her oral health as treatment progressed. One thing that really bothered me during treatment was that I found four carious lesions and C.K. had just been to the dentist to have X-rays taken about three months prior. When I asked her, she said that the dentist did not tell her about the cavities. I also noticed that the crown that she had on tooth #30 was ill-fitted and it was causing the gingiva in that area to become very inflamed, flaccid and puffy. I was pleased to learn that since that particular visit, the patient has changed dentists.
This patient’s gingival tissue improved as treatment progressed. Initially, the gingiva had red, rolled margins, was inflamed, whitish and soft. By the patient’s final visit, the gingiva was more pink, firmer and more resilient as well as less inflamed.
There were no additional interventions developed with the patient as the treatment progressed.
REFLECTION
I think that with the use of a stronger anesthetic and more time (with a modified treatment plan to include more visits) that I could have had a more successful experience with this patient. It is possible that the next time that she returns for a cleaning, she will be a little more comfortable now that she knows what to expect.
Reflecting on my clinical treatment and faculty feedback, I think that the most positive experience for me was that since I was treating a family member, I felt good about being able to provide them with a service that is so essential to their overall health. Additionally, since I recognized the presence of caries and identified an ill-fitting crown, I was able to recommend that the patient find a new dentist. When the patient went to the dentist, she contacted me to let me know that my findings were correct. She did in fact have the caries and the crown has to be removed, to be replaced with an implant. It was immensely satisfying to have a patient confirm my findings with a dentist. I think that the patient will have more trust in my abilities and knowledge going forward.
Reflecting on my clinical treatment and faculty feedback, my clinical weakness that occurred during this session was that I treated the patient too fast. I should have increased the number of visits for this patient to ease their anxiety. I also struggled somewhat with instrumentation because this patient had a very small mouth. Because she was also very sensitive, moved around a lot and preferred to expectorate into a napkin instead of using suction or the sink, it was more difficult to treat her.
PREVENTION
My homecare plan was somewhat successful because the patient did practice the Modified Bass toothbrushing method and the anterior facial teeth exhibited much less plaque when her follow-up plaque score was taken. However, I should have had the patient incorporate the use of a child-sized toothbrush during the first visit when I demonstrated toothbrushing. I think that she would have embraced the whole experience much better. Regarding flossing, this patient is very used to floss gliders. She finds them easier to use than traditional floss. I explained to the patient that this type of floss is straight, so it only allows for an “up and down” motion while traditional floss can be curved to accommodate the anatomy of the teeth. However, if she is frustrated, I told her that she should continue to use the floss gliders instead of not flossing at all.
My stated outcomes were somewhat achieved because the patient’s plaque score went from poor to fair. The facial areas of her teeth exhibited reduced plaque. However, the lingual of her posterior teeth were still plaque-retentive. Using a smaller brush head should be able to improve this.
Using the gingival flipcharts in clinic to explain to the patient what plaque and biofilm are and how they can affect dental health was very effective with this patient. She was very curious and asked a lot of questions. Using the TRACE solution to color the areas that were plaque-retentive also worked very well with this patient. She wanted to see all of her teeth and noted where she was retaining the most plaque. My toothbrush recommendation did not initially work, which I modified at a later visit.
I was able to motivate my patient by discussing the active occlusal carious lesions present in her mouth. I explained to her that she had to concentrate on brushing these areas more, because this is where bacteria were building up. Using the analogy of bacteria invading, settling and creating a community amongst her teeth and gums also seemed to work when explaining to the patient how plaque leads to calculus. I really think that after this patient incorporates using a smaller brush head, she will find it much easier to practice good oral hygiene habits, especially in the posterior areas of her mouth.